Most people get vaccinated without any issues. But when someone has a serious allergic reaction after a shot, it makes headlines. And that’s understandable - it’s scary. But here’s the truth: vaccine allergic reactions are incredibly rare. Far rarer than being struck by lightning. The data doesn’t lie: for every million doses given, only about 1 to 2 people experience anaphylaxis - a severe, life-threatening allergic response. That’s less than 0.0002% of all vaccinations.
What Actually Counts as a Vaccine Allergy?
Not every rash, itch, or sore arm after a shot is an allergy. True allergic reactions are driven by the immune system overreacting to something in the vaccine. The most dangerous type is an IgE-mediated reaction - the kind that leads to anaphylaxis. Symptoms show up fast: hives, swelling of the lips or tongue, trouble breathing, a sudden drop in blood pressure. These usually happen within minutes, often within the first 15 minutes after the shot. But here’s what most people don’t realize: many reactions aren’t allergies at all. A fever, mild swelling at the injection site, or a delayed rash? Those are common side effects, not immune system overreactions. In fact, studies show that up to 13% of people report skin rashes after certain vaccines - but almost none of those are true allergies. They’re just the body’s normal response to being stimulated.What’s in the Vaccine That Could Cause a Reaction?
People often blame the virus component or the dead bacteria in vaccines. But those aren’t the culprits. The real triggers are the tiny, non-active ingredients added to make the vaccine stable or effective. Polyethylene glycol (PEG) is one of the most talked-about now. It’s used in mRNA vaccines like Pfizer and Moderna to protect the fragile genetic material. A small number of anaphylaxis cases after these vaccines have been linked to PEG allergies - but only in people who already had a known, severe PEG allergy before vaccination. If you’ve had anaphylaxis to PEG-containing products like some laxatives or IV fluids, talk to your doctor before getting an mRNA shot. Another common concern is egg. Years ago, people with egg allergies were told to avoid flu shots. That changed after decades of research. Studies tracked over 4,300 people with egg allergies - including 656 who had had life-threatening reactions to eating eggs - and gave them the flu vaccine. Not one had a serious allergic reaction. Today, no special precautions are needed for egg-allergic individuals. Yeast is another ingredient people worry about, especially in hepatitis B and HPV vaccines. But among nearly 200,000 allergy reports in the U.S. safety database, only 15 cases even hinted at yeast being involved. And in most of those, other causes couldn’t be ruled out. Aluminum salts, used as adjuvants to boost immune response, don’t cause anaphylaxis. But they can lead to persistent lumps under the skin - harmless, but sometimes alarming. These are not allergic reactions. They’re local tissue responses.Who’s Most at Risk?
Women make up over 80% of reported allergic reactions to vaccines. Why? It’s not fully understood, but similar patterns show up in other drug allergies. Age doesn’t matter much - reactions have been seen in babies as young as 3 months and adults over 80. The average age is around 40. The biggest risk factor? A history of severe allergies - especially anaphylaxis to any substance, not just vaccines. About 81% of people who had anaphylaxis after a vaccine had a prior history of serious allergic reactions. That’s why providers ask about your allergy history before giving shots. It’s not about the vaccine. It’s about your personal immune profile.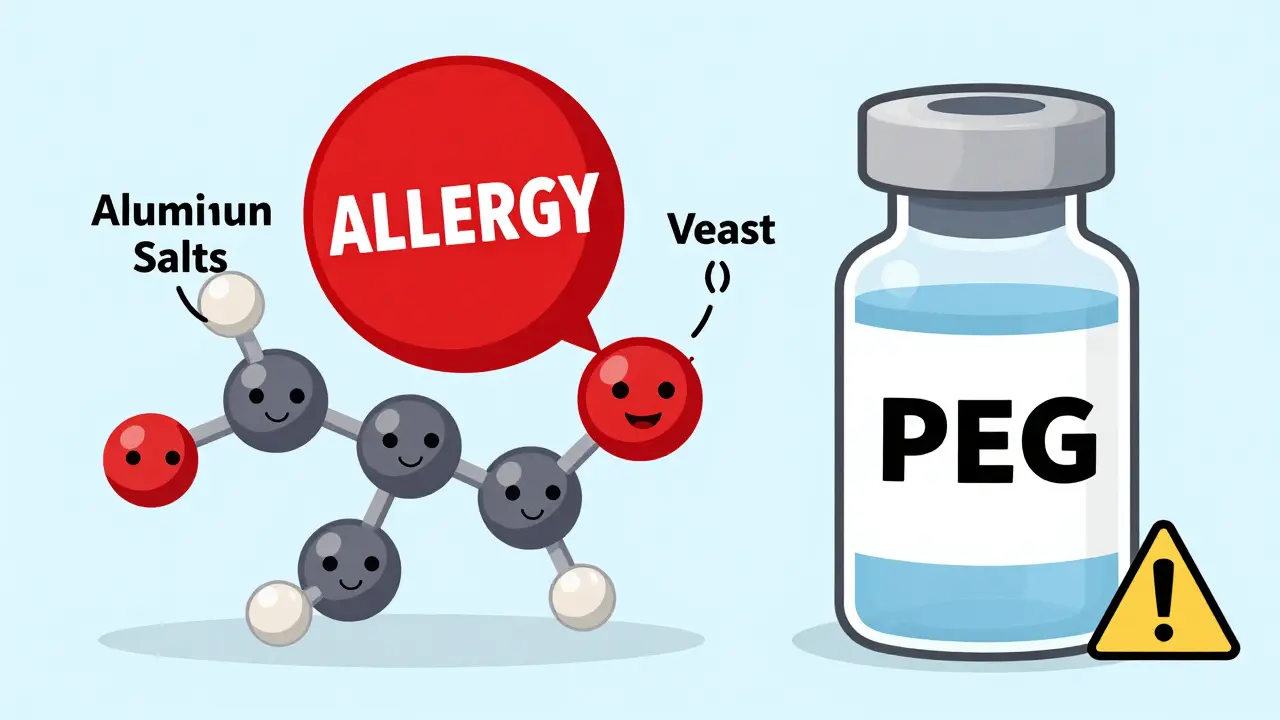
How Are These Reactions Monitored?
The U.S. has one of the most detailed vaccine safety systems in the world: VAERS - the Vaccine Adverse Event Reporting System. It’s run by the CDC and FDA. Anyone - doctors, patients, parents - can report a problem after a vaccine. It’s not a proof system. It’s a warning system. VAERS gets 30,000 to 50,000 reports a year. Most are minor. But when something unusual pops up - like a spike in a certain type of reaction - scientists dig in. They compare the numbers to expected background rates. If a pattern emerges, they launch deeper studies. During the COVID-19 rollout, the CDC added v-safe - a smartphone tool that texted people daily for a week after vaccination, then weekly for months. Over 3.6 million people used it. It helped catch the slight uptick in anaphylaxis rates with mRNA vaccines - from 1.3 per million to about 5 per million. That’s still extremely rare. But without v-safe, we might have missed it. Europe has EudraVigilance. Canada, Australia, Japan - all have similar systems. The goal? Catch problems early, before they become widespread.What Happens If You Have a Reaction?
All vaccination sites are required to have epinephrine on hand - the only medication that can stop anaphylaxis in its tracks. Staff must be trained to recognize it and act fast. The standard rule: watch everyone for 15 minutes after the shot. If you’ve had a previous allergic reaction to any vaccine or injection, stay for 30 minutes. If anaphylaxis happens, epinephrine is given immediately. Then, the person is transported to a hospital. Most recover fully with prompt treatment. In a study of over 10 million doses, zero deaths were linked to allergic reactions. Afterward, the reaction must be reported to VAERS. That’s not optional. It’s how we learn.