LAI Side Effect Monitoring Calculator
LAI Side Effect Monitoring Calculator
Calculate when your next side effect checks should be done based on your last injection date and medication type.
When a patient starts a long-acting injectable (LAI) antipsychotic, they’re not just getting a shot. They’re signing up for months of stable medication - but only if the side effects are watched closely. Too often, that monitoring doesn’t happen. In 2021, a major audit of UK mental health services found that only 45% of patients on LAIs had any documented side effect assessment in the past year. That’s not a minor oversight. It’s a systemic failure.
What Long-Acting Injectables Actually Do
Long-acting injectables aren’t just pills you don’t have to swallow. They’re specially formulated drugs - like paliperidone, aripiprazole, or olanzapine - that slowly release over weeks or even months. A single shot can replace daily pills, cutting down on missed doses and lowering relapse rates by 30-50%. That’s why their use has grown: the global market hit $5.8 billion in 2023 and is expected to keep rising. But here’s the catch: these drugs don’t just work longer. They also last longer in your body. That means side effects stick around too. And if you’re not checking for them regularly, they can turn serious - fast.The Hidden Risks No One Talks About
Most people think of LAIs as just helping with hallucinations or paranoia. But the real danger lies in what happens beneath the surface. Take paliperidone (Invega Sustenna). About 60-70% of users develop high prolactin levels, which can cause sexual dysfunction, breast growth, or missed periods. One in five develops metabolic syndrome - high blood sugar, belly fat, bad cholesterol - and 20-30% end up with type 2 diabetes. Yet, in the same UK audit, only 15% of patients had their blood sugar or lipids checked in the past year. Olanzapine LAI (Zyprexa Relprevv) has a black box warning. After each injection, patients must be monitored for three hours because of the risk of sudden sedation or delirium. There have been deaths linked to this. Still, many clinics skip the full observation window because it’s inconvenient. Even “safer” options like aripiprazole aren’t risk-free. Up to 25% of users get akathisia - a terrifying feeling of inner restlessness that makes people pace, rock, or feel like they can’t sit still. Left unchecked, it can lead to suicide risk. And then there’s tardive dyskinesia - involuntary movements in the face, tongue, or limbs. It can be permanent. The American Association of Psychiatric Pharmacists says you need to use the AIMS scale every three months. But in community clinics, many nurses say they’ve never been trained to do it properly.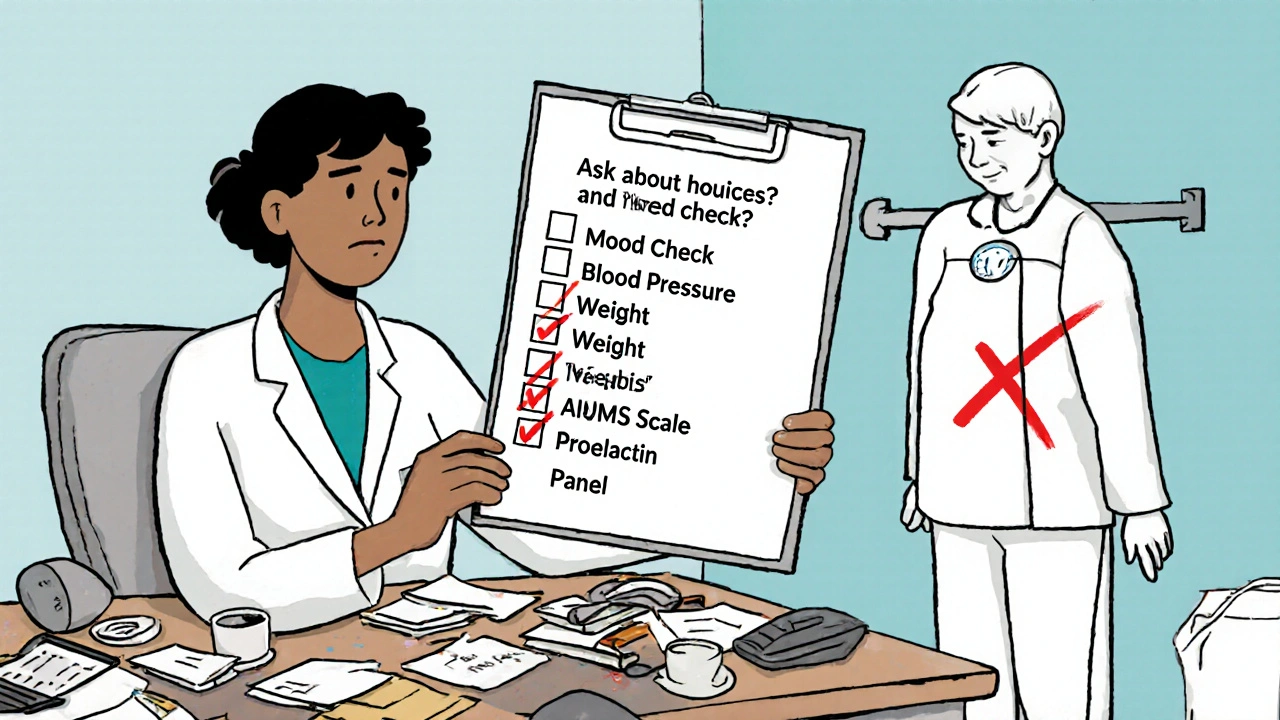
Why Monitoring Falls Through the Cracks
You’d think that with regular injection visits - every 2, 4, or 12 weeks - clinicians would have plenty of chances to catch problems. But time is the enemy. One community psychiatrist on Reddit said: “I have 15 LAI patients. Each appointment is 15 minutes. I prioritize symptoms because that’s what gets reimbursed.” Insurance systems pay for talking about voices or mood. They don’t pay for checking blood pressure, waist size, or prolactin levels. So those checks get pushed aside. Training is another issue. A 2023 survey of 200 mental health nurses found that 62% felt unprepared to monitor LAI side effects. Many only look for redness or swelling at the injection site. They don’t ask about weight gain, energy levels, or movement changes. Patients aren’t always aware either. One user on Schizophrenia.com shared: “I gained 30 pounds on Invega Sustenna over 18 months. My doctor never asked about my weight. He just asked, ‘How are you feeling mentally?’”What Good Monitoring Actually Looks Like
There’s a blueprint for doing it right. The National Council’s 2022 guide lays it out clearly:- Before every injection: Check vital signs (blood pressure, temperature, heart rate), ask about movement problems, weight gain, sexual changes, and injection site pain.
- After injection: Observe for 30 minutes (or 3 hours for olanzapine). Watch for dizziness, confusion, or fever.
- Every 3 months: Use the AIMS scale to screen for tardive dyskinesia.
- Every 6 months: Run a full metabolic panel - fasting glucose, cholesterol, triglycerides.
- Annually: Check prolactin levels if on paliperidone or risperidone.
New Tools Are Helping - But They’re Not Enough
Technology is stepping in. Some clinics now use smartphone apps that remind patients to log symptoms between visits. One pilot study showed a 30% increase in early detection of side effects. Telehealth check-ins for weight and blood pressure are being recommended by the American Psychiatric Association. There’s even a blood test in phase 2 trials (NCT05214587) that might predict who’s likely to gain weight on LAIs before they even start. If it works, it could change everything. But these tools aren’t widespread. And they can’t replace a clinician asking the right questions.The Bottom Line: Monitoring Isn’t Optional
LAI antipsychotics are powerful. They give people stability. But that stability only lasts if we pay attention to the whole body - not just the mind. The data is clear: without structured, consistent side effect monitoring, LAIs become a ticking time bomb. Weight gain leads to diabetes. High prolactin leads to bone loss. Tardive dyskinesia leads to shame and isolation. Neuroleptic malignant syndrome - rare, but deadly - can strike without warning. We’re not talking about minor discomforts. We’re talking about preventable, life-altering, sometimes fatal outcomes. The solution isn’t more drugs. It’s better care. Clinics need time. Staff need training. Systems need to pay for it. Patients need to be told: your body matters just as much as your mind. Until then, the 45% documentation gap isn’t just a statistic. It’s a warning.Are long-acting injectables safer than oral antipsychotics?
They’re not inherently safer - they just improve adherence. The same side effects exist, but because the drug stays in your system longer, problems can build up unnoticed. Without regular monitoring, LAIs can actually increase the risk of long-term complications like metabolic syndrome or tardive dyskinesia.
How often should side effects be checked for LAIs?
At every injection visit, vital signs and injection site reactions should be checked. Movement disorders (like tardive dyskinesia) need assessment with the AIMS scale every 3 months. Blood sugar, cholesterol, and weight should be tracked every 6 months. Prolactin levels should be tested every 6-12 months if on paliperidone or risperidone. High-risk patients need more frequent checks.
Why is olanzapine LAI different from other LAIs?
Olanzapine LAI carries a FDA black box warning for post-injection delirium/sedation syndrome (PDSS), a rare but life-threatening reaction. Patients must be monitored for 3 hours after each injection. This requirement doesn’t exist for other LAIs. It’s the most intensive monitoring protocol of any antipsychotic injection.
Can patients monitor their own side effects?
Patients can track symptoms like weight gain, mood changes, or movement issues using apps or journals, but they can’t replace clinical assessments. Blood tests, AIMS evaluations, and vital sign checks require trained staff. Patient reporting helps catch early signs, but professional monitoring is still essential.
What happens if side effects go undetected?
Undetected side effects can lead to irreversible damage: type 2 diabetes, heart disease, permanent movement disorders, or even death from neuroleptic malignant syndrome. They can also cause patients to stop treatment because they feel worse - not because the drug isn’t working, but because the side effects weren’t managed.
Are there guidelines for LAI monitoring?
Yes. The Royal College of Psychiatrists, the American Association of Psychiatric Pharmacists, and the National Council all publish detailed guidelines. They recommend quarterly movement disorder assessments, biannual metabolic panels, and immediate post-injection observation for high-risk drugs like olanzapine LAI. But adoption remains inconsistent across clinics.
Is LAI monitoring covered by insurance?
Most insurance plans cover the injection itself and basic psychiatric visits, but they rarely reimburse for time spent on physical health monitoring like blood tests, weight checks, or AIMS assessments. This creates a financial disincentive for providers to do thorough monitoring - even though it reduces long-term costs by preventing hospitalizations.
What’s being done to improve LAI monitoring?
Some Medicare Advantage plans now include LAI monitoring metrics in their quality incentive programs. The FDA is considering expanding REMS requirements to other high-risk LAIs. Digital tools and telehealth are being integrated. And a global consortium is pushing for standardized monitoring protocols by 2026. But progress is slow without funding and training.





November 25, 2025 AT 07:51 AM
Man, I’ve seen this play out in my brother’s care team-every visit is rushed, and the only thing they check is if he’s ‘doing better mentally.’ No weight, no bloodwork, no AIMS scale. He gained 50 pounds in a year and didn’t even realize it was the meds until his diabetes diagnosis. It’s not negligence-it’s a system designed to ignore the body.
November 26, 2025 AT 09:21 AM
I work in a community clinic and we’re trying to build a checklist into our EHR. It’s slow, but we started with just 3 things: weight, BP, and ‘any new shaking or restlessness?’ One nurse said it changed her whole approach-she finally felt like she was seeing the whole person. Small steps, right?
November 26, 2025 AT 22:20 PM
45% documentation rate? That’s not an oversight. It’s a scandal.
November 27, 2025 AT 22:18 PM
Bro, this is wild. I didn’t even know olanzapine LAI needs 3 hours of observation 😳 I thought it was just like the other shots. My cousin got it last month and they let her leave after 20 mins. Like… what?!?! We need to stop treating mental health like it’s just about thoughts. The body is part of the brain too 💪🧠
November 28, 2025 AT 07:06 AM
Let me be clear: if your clinic isn’t doing AIMS every 3 months, they’re not doing their job. It’s not optional. It’s not ‘nice to have.’ It’s a standard of care. If you’re not tracking tardive dyskinesia, you’re not just being lazy-you’re risking permanent damage. And yes, that’s on you if you’re the provider.
November 29, 2025 AT 22:41 PM
There’s a reason why people stop these meds-not because they don’t work, but because they feel worse and no one asks why. I’ve seen patients quit because they were too embarrassed to say they had breast growth or couldn’t have sex. We need to normalize asking those questions. Like, just say it. ‘Hey, how’s your libido?’ It’s not awkward. It’s medical.
December 1, 2025 AT 19:59 PM
So you’re telling me we’re giving people drugs that can cause diabetes and permanent movement disorders… and we don’t even test their blood? What is this, 1950? You people are pathetic. Just give them pills. At least then they can forget to take them and die on their own time. This is just corporate medicine with a fancy injection.
December 3, 2025 AT 01:15 AM
The real tragedy isn’t the 45% documentation rate-it’s that we’ve turned healing into a transaction. We’ve forgotten that a human being is not a data point. We’re not just treating psychosis-we’re holding souls together with syringes and spreadsheets. And when the soul screams, no one hears it because the billing code doesn’t exist.
December 3, 2025 AT 12:53 PM
Just had a chat with a nurse in Perth who said they started using a simple Google Form for patients to log symptoms between visits. Turns out, people are way more honest when it’s anonymous. One guy admitted he was pacing all night-turned out to be akathisia. Saved him from a suicide attempt. Tech ain’t perfect, but it’s a start.
December 3, 2025 AT 15:15 PM
My sister’s on LAI and we started doing monthly weight checks at home. She hates it, but now she sees the trend. Last month she said, ‘I think I need to talk to my doctor.’ That’s the win. You don’t need a whole team. You just need someone who cares enough to notice.
December 4, 2025 AT 00:47 AM
I’ve been a nurse for 12 years and I’ve never been trained on AIMS. No one ever showed me how to do it. I just check the injection site and ask if they’re feeling okay. If they say yes, we move on. This article made me cry. We’re not bad people-we’re just broken by the system.