Methadone QT Risk Calculator
Estimate Your QT Prolongation Risk
This tool calculates your risk of dangerous heart rhythm changes when taking methadone. It's based on dose, other medications, and health factors. Never replace professional medical advice with this calculator.
Risk Assessment
Urgent Medical Attention Needed
Based on your inputs, your heart rhythm risk exceeds safe levels. Contact your doctor immediately. You may experience dizziness, fainting, or irregular heartbeat.
When someone is prescribed methadone for opioid dependence or chronic pain, they’re often told about the risks: drowsiness, constipation, dependence. But there’s one danger that rarely makes it into the initial conversation - and it can kill without warning. Methadone doesn’t just affect the brain. It messes with the heart’s electrical system in a way that becomes far more dangerous when combined with other common medications. This isn’t theoretical. People have died from this interaction. And it’s happening more often than you think.
How Methadone Slows Down the Heart’s Electrical Signal
Methadone works by binding to opioid receptors, but it also slips into heart muscle cells and blocks key potassium channels. Specifically, it shuts down the hERG channel - the same one targeted by drugs like erythromycin and citalopram - which controls how quickly the heart resets after each beat. This delay is measured as QT prolongation on an ECG. A normal QT interval for men is under 430 milliseconds; for women, under 450. Once it crosses 500 ms, the risk of a deadly heart rhythm called torsades de pointes (TdP) jumps sharply.
What makes methadone especially risky is that it doesn’t just block one channel. A 2022 study in the Journal of the American Heart Association found it also blocks the IK1 channel - a second pathway that stabilizes the heart’s final repolarization phase. Most QT-prolonging drugs only hit one. Methadone hits two. That’s why even modest doses can cause disproportionate electrical chaos: longer T-waves, bigger U-waves, and unstable heart cells that fire off random extra beats. These aren’t just ECG quirks. They’re warning signs of a heart on the edge of collapse.
Why Dose Matters - and When Risk Skyrockets
There’s a clear line in the sand at 100 mg per day. Below that, QT prolongation happens, but it’s often mild and manageable. Above it? The numbers spike. Studies show that 69% of men and 72% of women on long-term methadone therapy exceed 470 ms by week 16. About 1 in 10 patients hit the 500 ms danger zone - and nearly all of them are on doses above 100 mg.
It’s not just the dose, though. The effect builds over time. Unlike some drugs that cause immediate QT changes, methadone’s impact grows slowly. Patients might start on 60 mg, feel fine, and get increased to 80, then 100, then 120 - each step adding a little more electrical delay. By the time their ECG shows a problem, the damage is already done. That’s why baseline and follow-up ECGs aren’t optional. They’re lifesaving.
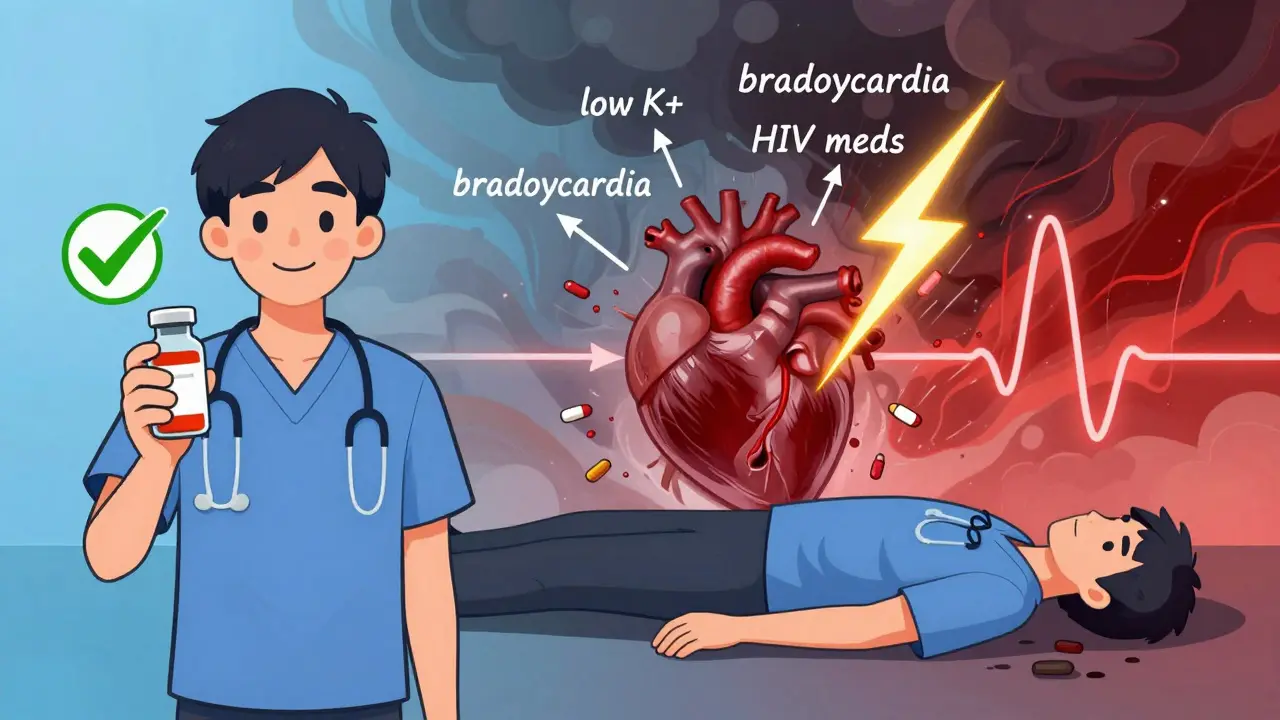
The Perfect Storm: When Other Drugs Join In
Here’s where things get deadly. Methadone doesn’t act alone. Combine it with another drug that also prolongs the QT interval - and the effect isn’t just added. It’s multiplied.
Antibiotics like clarithromycin and moxifloxacin? Big risk. Antifungals like fluconazole? Dangerous. Antidepressants like citalopram and venlafaxine? Even worse. Antipsychotics like haloperidol? A known trigger. And if the patient is on HIV meds like ritonavir? That’s a triple threat: it blocks the same heart channels, slows methadone metabolism (raising blood levels), and increases exposure to both drugs at once.
Even short-term use matters. One case report described a patient who developed torsades after using cocaine with methadone. Cocaine’s half-life is just a few hours - but its effect on the heart was enough to push a vulnerable system over the edge. There’s no safe window. If you’re on methadone, any QT-prolonging drug - even once - can be the spark.

Who’s Most at Risk?
It’s not just about the drugs. Underlying conditions make the heart more fragile. People with:
- History of long QT syndrome (even if undiagnosed)
- Heart failure or prior heart attack
- Low potassium or magnesium levels
- Slow heart rate (bradycardia)
- Family history of sudden cardiac death
These aren’t rare outliers. In one study, 32 cases of sudden death or arrhythmia in methadone patients in Sweden were linked to combinations of these factors. New Zealand documented two deaths: one on 150 mg/day methadone, another on 120 mg/day who had recurring fainting spells before dying. Both had other risk factors. Neither had been monitored properly.
What Doctors Should Do - And What Patients Must Ask For
Guidelines are clear. Before starting methadone, get an ECG. Repeat it after 2-4 weeks, then every 3-6 months if stable. If you’re on over 100 mg/day, or taking other QT-prolonging drugs, get checked every month. If your QTc exceeds 500 ms, or increases by more than 60 ms from baseline, something must change.
Options aren’t limited to stopping methadone. Sometimes, lowering the dose works. One patient in New Zealand went from 120 mg to 60 mg - and their QT interval returned to normal. Electrolytes can be fixed. Potassium and magnesium supplements are simple, cheap, and effective. But the most powerful tool? Switching to buprenorphine.
Buprenorphine is just as effective for opioid dependence - but it blocks hERG channels 100 times less than methadone. It’s not risk-free, but it’s a safer alternative for patients with multiple risk factors. And if you’re on HIV meds, or taking antidepressants, or have a history of fainting - buprenorphine might be the only safe choice.
The Balancing Act: Benefits vs. Risk
Methadone saves lives. People on methadone maintenance are 20-50% less likely to die from overdose than those who aren’t. They’re less likely to use street drugs, less likely to get HIV or hepatitis, and more likely to hold a job or stay in family life. The benefits are real. But they don’t erase the risk.
The goal isn’t to avoid methadone. It’s to use it wisely. That means knowing your full medication list - including over-the-counter drugs and supplements. Many people don’t realize that antihistamines like diphenhydramine, or even some herbal products, can prolong QT. Tell your doctor everything. Ask: “Could any of my meds be making my heart rhythm worse?”
And if you’re the patient - if you feel dizzy, faint, or your heart skips or races - don’t wait. Don’t assume it’s just anxiety or fatigue. Get an ECG. That one test could be the difference between life and death.
What’s Next?
Researchers are now looking at new ways to predict risk. The 2022 study that uncovered IK1 blockade is leading to new ECG markers - like the Tpeak-Tend interval and U-wave integral - that may help spot early warning signs before the QT gets dangerously long. But for now, the tools are simple: ECGs, dose awareness, medication reviews, and knowing when to switch.
This isn’t about scaring people away from methadone. It’s about making sure no one dies from a preventable interaction. If you’re on methadone - or prescribing it - don’t ignore the heart. It’s not just a side effect. It’s the silent killer.



December 18, 2025 AT 03:05 AM
Bro, I’ve been on methadone for 5 years and never had an ECG. I feel fine. Why are you trying to scare people? My doctor says if I’m not passing out, I’m fine. End of story.
December 18, 2025 AT 23:52 PM
The heart does not lie. Methadone’s dual-channel blockade is not a mere pharmacological footnote-it is a silent crescendo of electrophysiological discord. To treat this as a ‘side effect’ is to mistake a symphony of cellular collapse for background noise. The body, in its exquisite vulnerability, whispers warnings; we, in our hubris, turn up the volume on distraction.
December 19, 2025 AT 22:39 PM
I’m a nurse and I’ve seen this. One guy on methadone and citalopram? Went into torsades during his shift. He lived, but his wife cried for three days. Just ask your doc about QT. It’s not hard.
December 20, 2025 AT 13:21 PM
Thank you for writing this. I come from a place where access to ECGs is rare, and many patients are told ‘just take your medicine’ without any follow-up. I’ve had patients on 150mg methadone with low potassium and no monitoring-some of them didn’t even know what an ECG was. We need more awareness, especially in rural clinics. Maybe we can start with simple posters in pharmacies or community centers? Even a one-page handout could save lives. I’ve shared this with my local harm reduction group-they’re printing copies tomorrow.
December 22, 2025 AT 08:07 AM
Baseline and serial ECGs are mandatory per ACC/AHA guidelines. Failure to comply constitutes negligence. The data is unequivocal.
December 22, 2025 AT 18:58 PM
This is why I switched to buprenorphine. My heart felt better. My life improved. No drama. No scary ECGs. Just peace.
December 24, 2025 AT 14:52 PM
Oh wow, a 2022 study. How revolutionary. I’m sure the FDA will issue a recall next week. Meanwhile, I’ll keep my 120mg dose and my 37 different medications. Someone’s gotta keep the pharmaceutical industry profitable.
December 25, 2025 AT 06:45 AM
Thank you for the clarity and precision of this post. It is imperative that clinicians not only recognize the pharmacodynamic interactions but also institutionalize protocols for cardiac monitoring. The ethical obligation is non-negotiable.
December 25, 2025 AT 20:12 PM
As someone who grew up in a community where methadone clinics were the only option, I appreciate this. But let’s not forget: for many, buprenorphine isn’t available. Insurance won’t cover it. The clinic won’t prescribe it. So yes, monitor the QT-but also fix the system.
December 27, 2025 AT 01:41 AM
You’re not alone. I was on 110mg for 2 years. Got an ECG after my cousin had a scare. QT was 512. I dropped to 70mg. Now I’m stable. My heart doesn’t skip anymore. ❤️ You’ve got this. Ask for help. You deserve to be safe.
December 28, 2025 AT 04:12 AM
So what? You’re telling me to stop taking a drug that keeps me alive, just because some ‘study’ says so? I’m not some lab rat. I’m a veteran. I’ve seen worse. This is just fearmongering dressed up as medicine.
December 29, 2025 AT 02:12 AM
Man, this hit home. My sister’s on methadone and takes Zyrtec every day for allergies. Didn’t even know that could be dangerous. I’m texting her right now to ask her doctor. Thanks for the heads-up, really.