When you’ve had a severe reaction to a medication, your body isn’t just saying "no" to that one pill-it might feel like it’s saying no to the whole family. But here’s the truth: not every reaction means you need to avoid every drug in that class. Too many people walk around with a label like "penicillin allergic" or "sulfa allergic"-and then get stuck with less effective, more expensive, or riskier alternatives. The real question isn’t just "what happened?" It’s why it happened, and whether the risk repeats across similar drugs.
What Counts as a Severe Drug Reaction?
A severe drug reaction isn’t just a rash or upset stomach. The FDA defines it as something that’s life-threatening, requires hospitalization, causes lasting disability, or leads to birth defects. In real terms, that means: anaphylaxis (trouble breathing, swelling, dropping blood pressure), Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), or DRESS syndrome (fever, rash, organ damage). These aren’t side effects-they’re emergencies. TEN alone kills 30 to 50% of people who get it. If you’ve had one of these, you need to take immediate, serious action.But here’s where most people get it wrong: 80 to 90% of reported drug reactions aren’t allergic at all. They’re predictable side effects-like nausea from antibiotics or stomach bleeding from NSAIDs. These don’t mean you’re allergic. They mean the drug doesn’t agree with your body. And that’s a very different situation.
True Allergies vs. Side Effects: The Key Difference
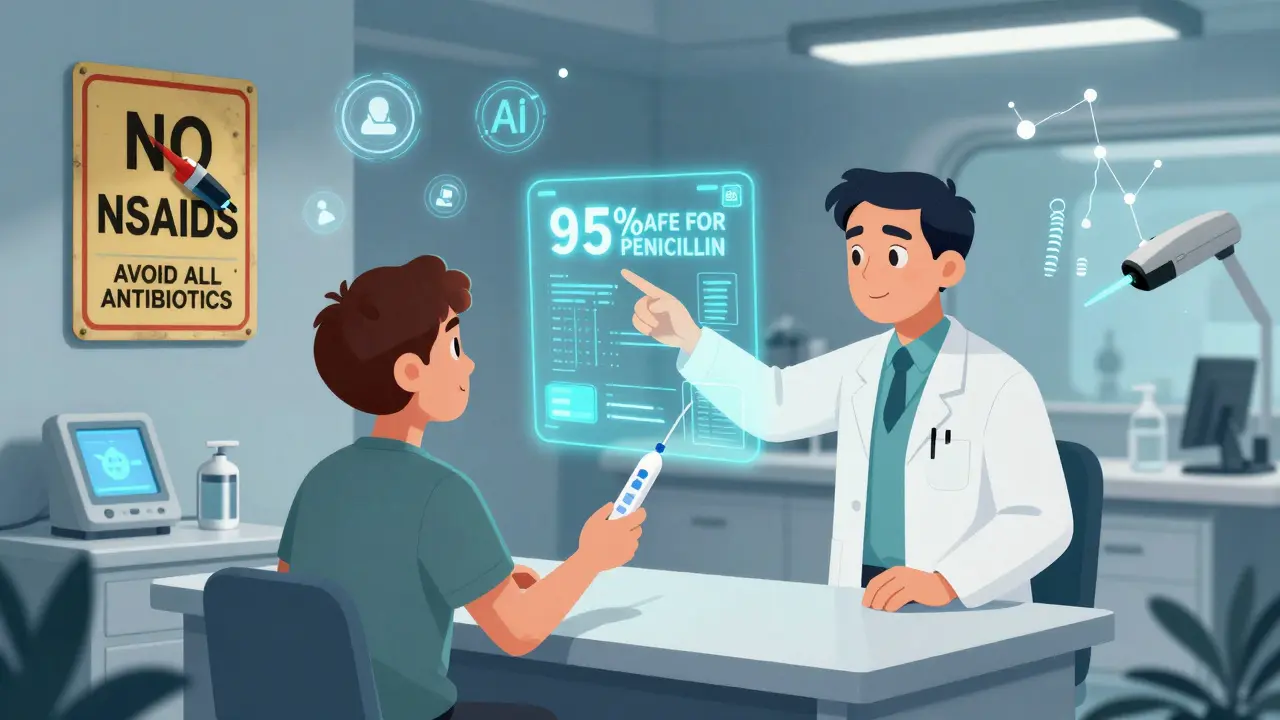
True allergic reactions involve your immune system. They usually show up fast-within minutes to hours. Symptoms include hives, swelling of the lips or tongue, wheezing, or anaphylaxis. These are IgE-mediated, and they’re dangerous because they can happen again, even with tiny amounts. If you’ve had anaphylaxis to penicillin, avoiding all beta-lactam antibiotics is usually the right call.But if you got a mild, itchy rash a week after taking amoxicillin? That’s likely not an allergy. Studies show 95% of people labeled "penicillin allergic" based on a childhood rash can actually take penicillin safely. That rash? It was probably a viral infection, not the drug. Yet most doctors still avoid all penicillin-family drugs out of caution. That’s unnecessary-and risky. You might end up on a broader-spectrum antibiotic that increases your chance of C. diff infection or antibiotic resistance.
Drug Families with High Cross-Reactivity Risks
Some drug families are more likely to cross-react than others. Here’s where caution is non-negotiable:- Beta-lactams (penicillins, cephalosporins, carbapenems): Cross-reactivity between penicillin and cephalosporins is only 0.5-6.5%, depending on the specific drugs. But if you had anaphylaxis to amoxicillin, you should avoid all beta-lactams until tested.
- Sulfa antibiotics (Bactrim, sulfasalazine): True sulfa allergy affects about 3% of people. But if you had SJS or TEN from Bactrim, avoid all sulfonamide antibiotics. Non-antibiotic sulfa drugs (like some diuretics or diabetes meds) are chemically different and usually safe.
- NSAIDs (ibuprofen, aspirin, naproxen): If you have aspirin-exacerbated respiratory disease (AERD), 70% of you will react to other NSAIDs. But if you just got a stomach ache from ibuprofen, switching to celecoxib (a COX-2 inhibitor) is often fine.
- Anticonvulsants (carbamazepine, phenytoin): These are top culprits in SJS/TEN. If you had a severe skin reaction to one, avoid the whole class. Genetic testing for HLA-B*15:02 (for carbamazepine) can prevent this in high-risk populations.
- Allopurinol: Causes DRESS in about 1 in 1,000 users. If you had it, never take allopurinol again-and avoid febuxostat cautiously, as some cross-reactivity exists.

When You Don’t Need to Avoid the Whole Family
You don’t need to throw out an entire drug class just because one drug in it caused trouble. Here’s when you can still use others:- Statin-induced muscle pain: Only 10-15% of people who react to one statin react to another. Switching from atorvastatin to rosuvastatin often works.
- GI upset from antibiotics: If amoxicillin gave you diarrhea, cephalexin might not. Different drugs, same class-different side effect profiles.
- Headache from a blood pressure med: If lisinopril made you cough, try a different ACE inhibitor or switch to an ARB like losartan. These are different mechanisms.
Doctors often default to avoidance because it’s easier than figuring out the details. But that’s not patient-centered care. It’s overcaution that harms.
The Danger of Over-Avoidance
Avoiding entire drug families without proof can cost you more than just convenience. A 2022 survey by the Asthma and Allergy Foundation found that 42% of people with drug allergy labels faced treatment delays-on average, 3.2 days longer than needed. That means longer illness, more hospital visits, and higher risk of complications.One patient on Drugs.com said: "After my Stevens-Johnson reaction to Bactrim, I got a UTI and was denied every antibiotic. They gave me a last-resort IV drug that cost $1,200 and left me in the hospital for a week. I just needed a simple oral antibiotic."
Meanwhile, research shows that 95% of people labeled "penicillin allergic" can tolerate it after proper testing. Yet most never get tested. Why? Because the system doesn’t prioritize it. Your allergy label might be outdated, wrong, or based on a misdiagnosed rash.
What You Should Do After a Severe Reaction
If you’ve had a severe reaction, follow these steps:- Get the details. Write down: What drug? When did symptoms start? What were they? Did you need epinephrine or hospitalization? This isn’t just for your records-it’s for your life.
- Use precise language. Don’t say "I’m allergic to penicillin." Say: "I had anaphylaxis 20 minutes after taking amoxicillin, with swelling and trouble breathing." Specificity saves lives.
- Ask about testing. Skin testing or blood tests (like ImmunoCap) can confirm true IgE-mediated allergies. For non-allergic reactions, a supervised drug challenge might be safe.
- Request a specialist referral. An allergist or immunologist can help you sort out what’s real and what’s not. Many hospitals now have drug allergy clinics.
- Update your records. Make sure your EHR has accurate, detailed allergy info. Poor documentation leads to dangerous overrides-23% of hospital alerts are ignored because the info is too vague.
And if you’ve been told you can’t take a drug family-ask: "Is this based on proof, or just caution?"
The Future: Precision Avoidance
The field is changing. Genetic testing now prevents reactions before they happen. HLA-B*57:01 testing for abacavir (an HIV drug) has cut hypersensitivity from 5% to less than 0.1%. The FDA approved a new diagnostic test in 2022 that’s 89% accurate-up from 60% for old skin tests. AI tools at places like Mayo Clinic are cutting inappropriate avoidance by 41%.But none of this matters if you don’t speak up. You’re your own best advocate. If you had a severe reaction, don’t accept a blanket avoidance without asking: "Could I be tested? Is there a safer option?"
Medication families aren’t all the same. Reactions aren’t all the same. And avoiding a whole class just because one drug hurt you might be doing more harm than good.



January 17, 2026 AT 16:52 PM
i got a rash from amoxicillin in 2012 and now i can't get any antibiotics without a fight. turns out it was just a virus. my doctor never tested me. now i'm stuck with cipro like a villain in a bad movie.
January 18, 2026 AT 09:21 AM
Oh wow. Someone actually wrote a 2000-word essay on something every med student learns in week two. Congrats, you've discovered that not all drug reactions are allergies. The real tragedy? You think this is news. 🙄
January 19, 2026 AT 05:27 AM
This is so important. I had a friend who avoided all NSAIDs because of a stomach ache from ibuprofen. Then she got chronic pain and couldn't take anything. Got tested, turned out she was fine. Changed her life. Always ask why.
January 21, 2026 AT 04:06 AM
MY SISTER HAD TEN FROM SULFA. SHE SPENT 6 MONTHS IN THE HOSPITAL. HER SKIN PEELING OFF LIKE WET PAPER. NOW YOU WANT ME TO JUST 'TRY ANOTHER DRUG'? ARE YOU OUT OF YOUR MIND? THIS ISN'T A MENU. THIS IS LIFE OR DEATH.
January 21, 2026 AT 09:33 AM
Big Pharma doesn't want you to know this. They profit from you being allergic to everything. That's why they don't fund testing. The FDA is in their pocket. You think this is medicine? It's a money racket. Wake up.
January 23, 2026 AT 07:53 AM
Yessss. I got labeled penicillin-allergic after a rash at 5. Turned out it was chickenpox. Got tested at 28. Now I take amoxicillin like it's candy. Why didn't anyone test me before? 😅
January 25, 2026 AT 01:52 AM
Reading this felt like someone finally put into words what I’ve been screaming at my doctors for years. I had a bad reaction to one statin, got told to avoid all of them. Switched to rosuvastatin - zero issues. Why do we treat medicine like a minefield instead of a toolbox?
January 25, 2026 AT 07:37 AM
so you're saying i should just randomly take drugs again after i almost died? wow. what a genius. maybe you should try living with the trauma before giving advice.
January 26, 2026 AT 20:18 PM
I had DRESS from allopurinol. I’m not touching anything in that class again. But I do wish my doctor had explained *why* it happened - not just told me to avoid everything. Knowledge helps you sleep at night.
January 27, 2026 AT 05:13 AM
people dont get it. its not about the drug. its about the energy. your body knows when something is wrong. you cant just test for it. the system is broken because they dont believe in soul medicine. i felt it in my bones when i took that pill. no test can measure that.
January 27, 2026 AT 05:21 AM
Why are we letting this happen in America? In Russia, they test everyone before prescribing. Here? You get a rash, you’re banned for life. We need mandatory allergy testing. No more guesswork. This is embarrassing.
January 29, 2026 AT 05:17 AM
Oh so now we're trusting 'tests' and 'allergists'? Next you'll tell me vaccines are safe and the moon landing wasn't faked. If your immune system says no, you don't argue with it. You listen. Science is just a story for people who like charts.
January 29, 2026 AT 19:25 PM
bro i had a rash from cephalexin and now i avoid ALL antibiotics. i'm not risking my glow up. 🧘♀️💊 #DrugAllergyLife #SquadGoals
January 31, 2026 AT 01:35 AM
Thank you for writing this. I’ve been afraid to ask for testing because I thought I’d sound dumb. Turns out, I just needed someone to say it’s okay to ask. I’m scheduling my skin test next week.
February 1, 2026 AT 15:11 PM
My mom got mislabeled penicillin allergic in the 70s. She never got tested. Last year she got pneumonia. They gave her azithromycin. She got sick again. Turned out she could’ve had amoxicillin. We lost so much time. This needs to change.