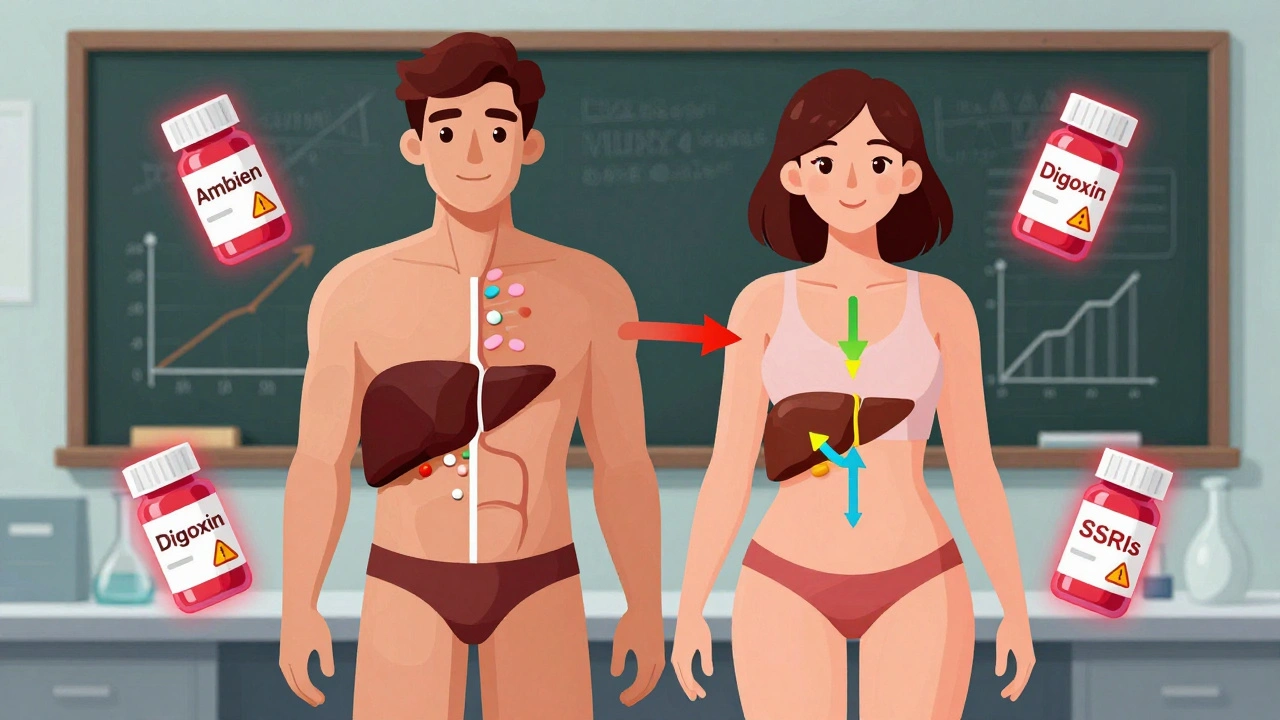
Women experience adverse drug reactions nearly twice as often as men due to biological differences and outdated clinical trial practices. Learn why dosing based on male physiology puts women at risk - and what’s being done to fix it.
Sex Differences in Drugs: How Gender Affects Medication Safety and Effectiveness
When it comes to how your body handles medicine, sex differences in drugs, how biological sex influences how medications are absorbed, processed, and eliminated by the body. Also known as gender-based pharmacology, it’s not just about hormones—it’s about liver enzymes, body fat, kidney function, and even stomach acid levels. A woman taking the same dose of a drug as a man isn’t just getting the same result. She might get stronger side effects, slower relief, or even no effect at all. This isn’t a theory—it’s been proven in studies of antidepressants, painkillers, heart meds, and even sleep aids.
Take drug metabolism, the process by which the body breaks down and eliminates medications. Women often have slower liver enzyme activity, especially CYP3A4 and CYP2D6, which means drugs like benzodiazepines or statins stick around longer. That’s why women are more likely to experience drowsiness from sleeping pills or muscle pain from statins. On the flip side, men tend to clear some drugs faster, which can lead to underdosing if prescriptions aren’t adjusted. Then there’s pharmacokinetics, how a drug moves through the body—absorption, distribution, metabolism, and excretion. Women generally have more body fat and less water, so fat-soluble drugs like antidepressants build up more easily. Meanwhile, kidney filtration rates are often lower in women, which affects how quickly drugs like antibiotics or blood pressure meds leave the system.
And it’s not just about chemistry. Women are more likely to be prescribed multiple medications at once, increasing the risk of dangerous interactions. They’re also more likely to report side effects, but those reports are often dismissed as "anxiety" or "overreaction." Meanwhile, clinical trials have historically used mostly male subjects, so many drug labels still don’t reflect how women respond. That’s changing slowly—but not fast enough. You need to know your body’s unique response to meds, especially if you’re on long-term treatment for heart disease, depression, or chronic pain. The sex differences in drugs aren’t a footnote—they’re a critical part of safe prescribing.
Below, you’ll find real-world examples from studies and patient experiences showing how these differences play out in daily life—from why women get more nausea from opioids to why men need higher doses of some antidepressants. These aren’t abstract concepts. They’re the reason someone might feel worse on a drug that "works for everyone." And if you’ve ever wondered why your medication didn’t work the same way for your sister, mom, or friend—this collection explains why.