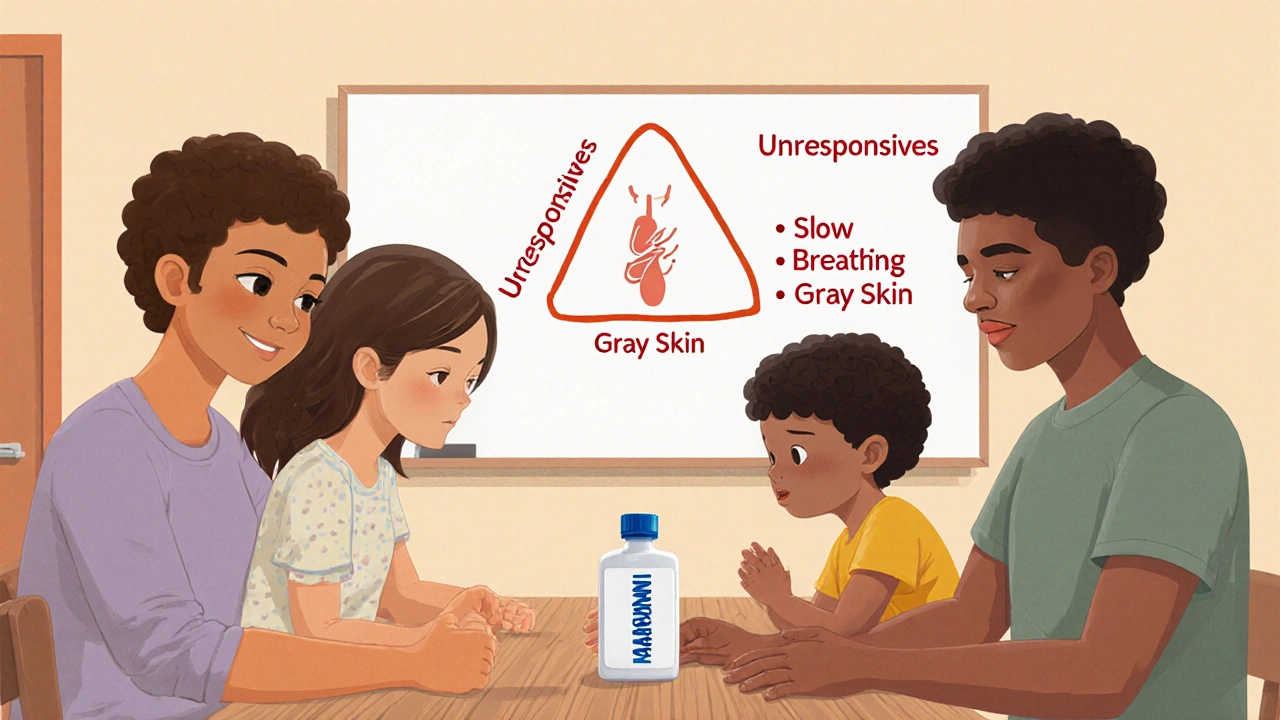
Learn how to teach your family to recognize overdose signs like unresponsiveness, slow breathing, and skin color changes. Includes step-by-step training methods, naloxone use, and real-life survival tips.
Overdose Symptoms: What to Watch For and When to Act
When someone takes too much of a drug—whether it’s prescription, over-the-counter, or illegal—their body can’t handle the load. This is called a drug overdose, a potentially life-threatening reaction to consuming more of a substance than the body can safely process. Also known as medication overdose, it doesn’t always look like what you see in movies. Sometimes it’s quiet. Sometimes it’s sudden. And if you don’t recognize the signs, it can turn deadly in minutes.
Not all overdoses are the same. An opioid overdose, a dangerous drop in breathing caused by drugs like heroin, fentanyl, or prescription painkillers often shows up as slow, shallow breaths, blue lips, and unresponsiveness. But an overdose symptom, any physical or mental change that signals the body is overwhelmed by a substance from something like acetaminophen or benzodiazepines can look completely different—nausea, confusion, irregular heartbeat, or even seizures. These signs don’t always appear together, and they can come on fast or hide for hours. That’s why knowing your meds and their risks matters more than ever.
Many people don’t realize how easily overdose symptoms can be missed. A tired friend who won’t wake up? Maybe they just slept too hard. A loved one vomiting after taking painkillers? Maybe they ate something bad. But if that person took more than the recommended dose—even by accident—those could be the first warning signs of something serious. The same goes for mixing medications. You won’t always know what’s in a pill you found, or how a supplement like Ginkgo biloba might react with your blood thinner. Overdose isn’t just about street drugs. It’s about the Tylenol you took with your cold medicine, the Xanax you doubled up on, or the leftover antibiotics you finished because you felt better.
What you’ll find in these posts isn’t just theory. It’s real-world insight from people who’ve lived through near-misses, caregivers who’ve learned the hard way, and experts who track how hidden risks show up after drugs hit the market. You’ll see how drug interactions—like beta-blockers hiding low blood sugar or acid reducers blocking absorption—can quietly push someone toward overdose. You’ll learn how counterfeit meds, like fake Ozempic or unregulated generics, carry unknown toxins that make overdose even more unpredictable. And you’ll find clear, no-fluff guidance on what to do if you spot the signs: call for help, stay with the person, and don’t wait for perfection.
This isn’t about fear. It’s about awareness. Because knowing the difference between a bad reaction and a true overdose can mean the difference between a hospital visit and a funeral. The tools to act are here. The signs are clearer than you think. You just need to know where to look.