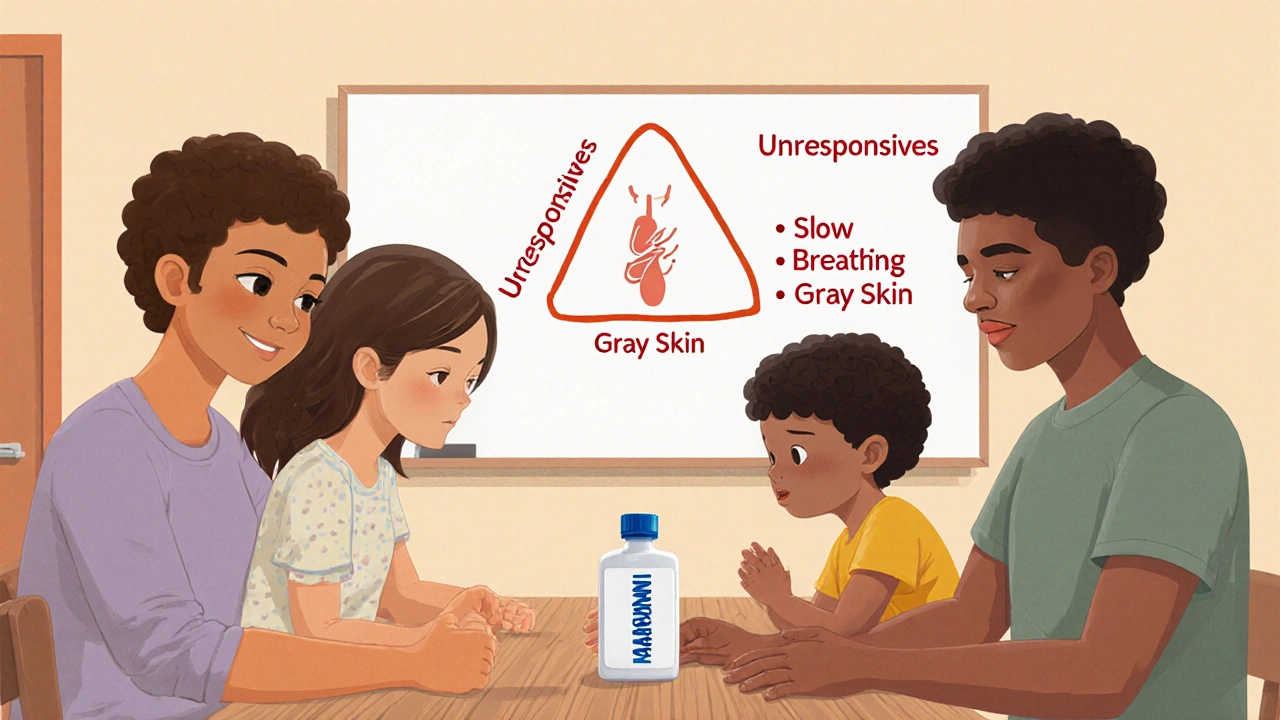
Learn how to teach your family to recognize overdose signs like unresponsiveness, slow breathing, and skin color changes. Includes step-by-step training methods, naloxone use, and real-life survival tips.
Opioid Overdose Signs: What to Recognize and Do Immediately
When someone is experiencing an opioid overdose, a life-threatening reaction caused by too much opioid in the body, often from prescription painkillers, heroin, or fentanyl. Also known as opioid poisoning, it shuts down breathing and can kill in minutes. This isn’t rare. In 2023, over 70,000 opioid-related deaths happened in the U.S. alone—and many of them were preventable if people knew what to look for.
The most dangerous sign is respiratory depression, when breathing slows to almost nothing or stops completely. You might notice slow, shallow breaths, or the person isn’t breathing at all. Their lips or fingernails turn blue or purple. They can’t wake up, no matter how much you shake or shout. Their skin feels cold and clammy. Pupils shrink to pinpoints. These aren’t side effects—they’re emergency signals. And they often happen fast, especially with fentanyl, which is 50 to 100 times stronger than morphine and sometimes mixed into other drugs without the user’s knowledge.
People often mistake an overdose for just being drunk or passed out. But if someone is unresponsive and breathing poorly, don’t wait. Don’t assume they’ll wake up. Don’t leave them alone. Call for help immediately. If you have naloxone, a medication that can reverse an opioid overdose within minutes. administer it right away—it’s safe, even if you’re not sure it’s an opioid overdose. Naloxone doesn’t work on alcohol, benzodiazepines, or stimulants, but it won’t hurt someone who doesn’t need it. Keep it handy if you or someone you know uses opioids, even if it’s prescribed.
Many overdoses happen alone. Someone takes a drug, doesn’t feel right, and can’t reach out. That’s why knowing these signs isn’t just helpful—it’s critical. Friends, family, even strangers can save a life by acting fast. You don’t need to be a doctor. You just need to know: no breathing? No response? Blue lips? That’s an overdose. Give naloxone. Call 911. Start rescue breathing if you’re trained. Every second counts.
The posts below cover real stories, medical facts, and practical advice about opioid risks, how naloxone works, why fentanyl is so dangerous, and what to do if someone you care about is struggling with dependence. You’ll find clear, no-fluff guidance from people who’ve been there—whether they’re patients, caregivers, or frontline responders. This isn’t theory. It’s survival knowledge. And it’s here because someone’s life might depend on it.