Heart failure management has transformed with new guidelines and medications. Learn how quadruple therapy, SGLT2 inhibitors, and monitoring devices help patients live longer and better-no matter the stage or type of heart failure.
HFpEF: Understanding Heart Failure with Preserved Ejection Fraction
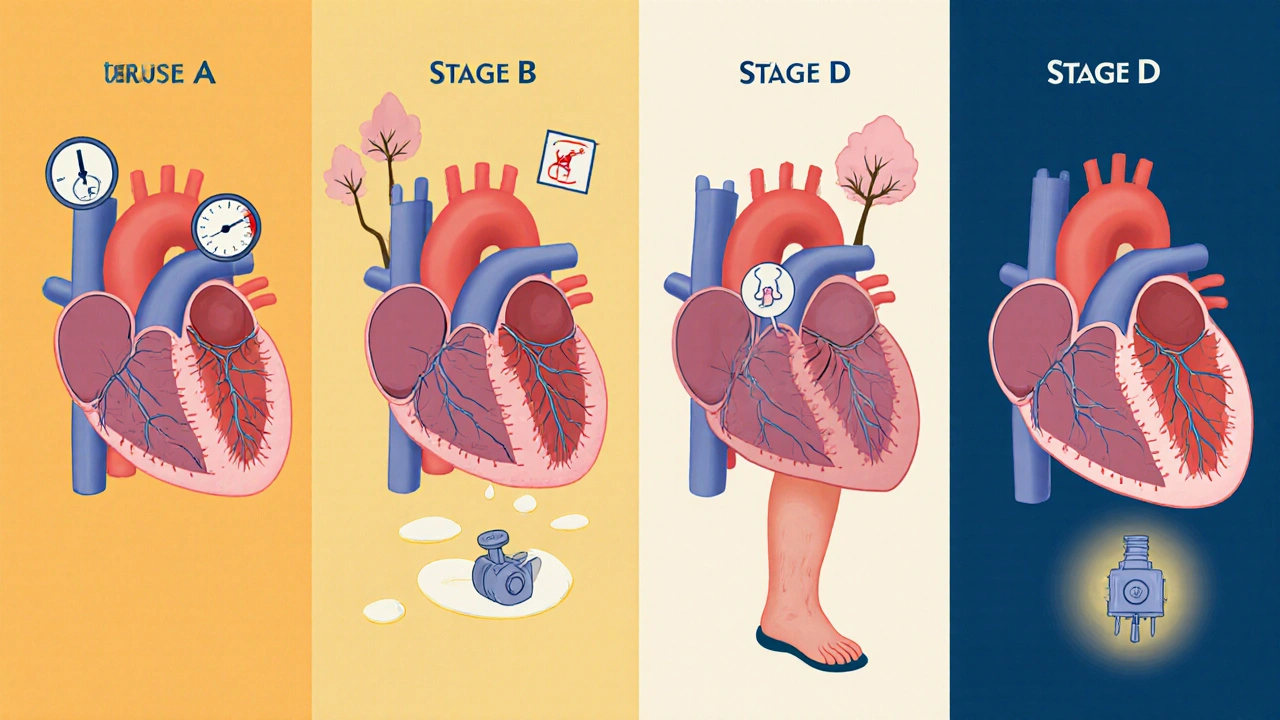
When your heart can't fill with enough blood between beats—even though it squeezes strongly—that's HFpEF, a form of heart failure where the left ventricle maintains normal pumping strength but becomes stiff and doesn't relax properly. Also known as diastolic heart failure, it's not a rare condition: nearly half of all heart failure cases in the U.S. are HFpEF, especially in older adults, women, and people with high blood pressure or diabetes. Unlike systolic heart failure, where the heart weakens and pumps poorly, HFpEF is about stiffness. The muscle thickens over time, often due to long-term strain from uncontrolled hypertension, obesity, or aging. This makes it harder for the heart to expand and take in blood, leading to fluid backup in the lungs and legs.
HFpEF doesn't show up on an echo as a weak pump, which is why it's often missed or misdiagnosed. Doctors look for signs like shortness of breath during light activity, swelling in the ankles, fatigue, and trouble lying flat. Blood tests for BNP or NT-proBNP, echocardiograms showing normal ejection fraction (usually over 50%), and signs of elevated pressure in the heart chambers help confirm it. What makes HFpEF tricky is that there's no single drug that fixes it. Unlike systolic heart failure, where ACE inhibitors or beta-blockers are standard, HFpEF treatment is more about managing the conditions that cause it—like controlling blood pressure, losing weight, and reducing fluid overload with diuretics. Recent studies show that SGLT2 inhibitors, originally diabetes drugs, now have solid evidence for improving outcomes in HFpEF patients, even without diabetes.
HFpEF is closely tied to other chronic conditions. If you have obesity, a major driver of inflammation and heart stiffness, or type 2 diabetes, which damages blood vessels and heart muscle over time, your risk goes up. Even chronic kidney disease, a common companion to HFpEF due to fluid and electrolyte imbalance makes it harder to manage. The good news? Lifestyle changes make a real difference. Losing just 5-10% of body weight can improve heart filling, lower blood pressure, and reduce symptoms. Regular walking, even 30 minutes a day, helps the heart become more flexible over time.
There's no cure yet, but understanding HFpEF means you're already ahead. The posts below cover real-world strategies—how to monitor symptoms at home, which medications actually help, why some common heart drugs don't work for this type of failure, and how to avoid dangerous interactions with other pills you might be taking. You'll find practical advice on managing fluid balance, recognizing warning signs before hospitalization, and working with your provider to build a plan that fits your life—not just your lab numbers.