Heart failure isn’t a single disease-it’s a cascade. It starts long before you feel short of breath. It begins with high blood pressure, a past heart attack, or even diabetes quietly damaging your heart over years. By the time fatigue and swelling show up, the heart has already been working harder than it should. But here’s the good news: we now have more tools than ever to stop it from getting worse-and even help you live better with it.
Understanding the Stages: It’s Not Just About Symptoms
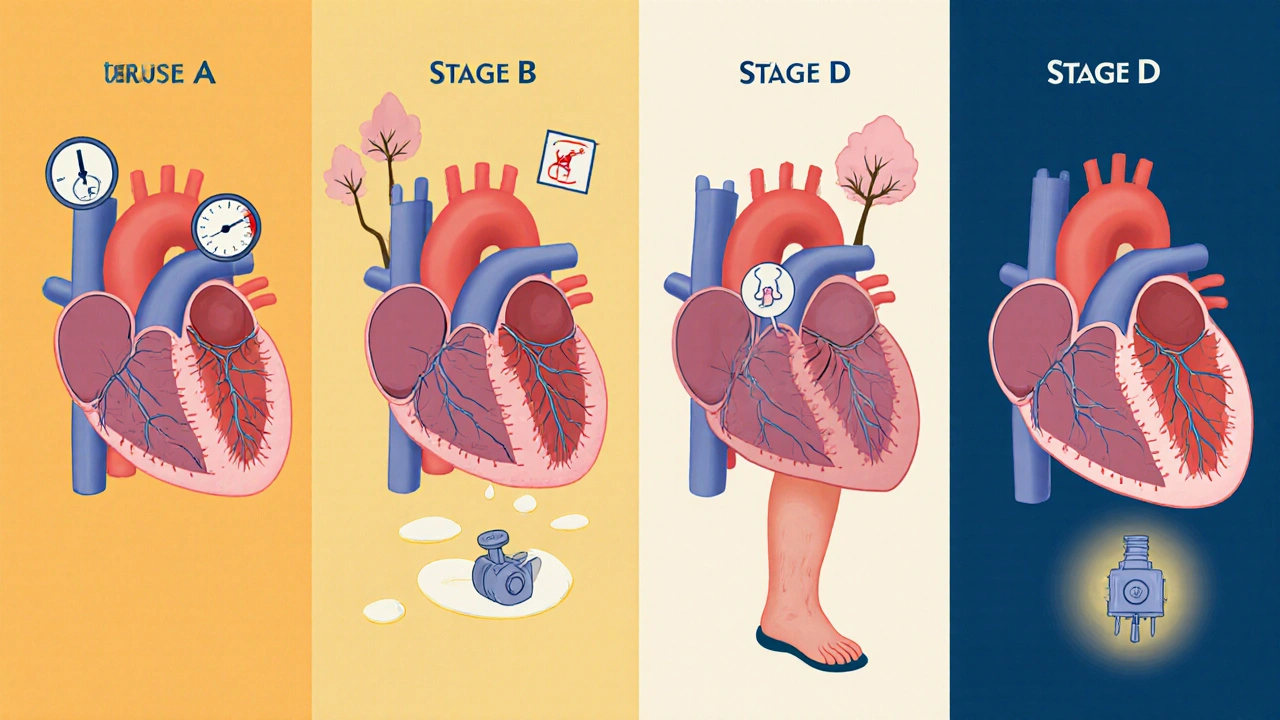
Doctors now classify heart failure in four stages, not just by how you feel, but by what’s happening inside your heart. Stage A means you’re at risk-maybe you have high blood pressure, diabetes, or a family history-but your heart still looks normal on an echo. Stage B is when damage has started: your heart is enlarged, or the wall is thickened, but you still have no symptoms. This is the critical window to act. Stage C is when symptoms appear-shortness of breath climbing stairs, swelling in your ankles, waking up gasping for air. Stage D is advanced: your heart is failing despite all treatments, and you need specialized care like a transplant or a mechanical pump.
What matters most isn’t just the stage, but your heart’s pumping ability. That’s measured by ejection fraction (EF)-the percentage of blood your left ventricle pushes out with each beat. If your EF is 40% or lower, you have HFrEF (heart failure with reduced ejection fraction). If it’s 50% or higher, you have HFpEF (heart failure with preserved ejection fraction). And if it’s in between, it’s called HFmrEF. For decades, HFpEF was seen as untreatable. Now, we have real options.
The New Standard: Quadruple Therapy for HFrEF
If you have HFrEF, the treatment has changed dramatically since 2023. The old approach was one or two pills. Now, the gold standard is four drugs, taken together. This isn’t theory-it’s backed by over 300 clinical trials and now the official guidelines from the American Heart Association and American College of Cardiology.
- ARNI (sacubitril/valsartan): Replaces ACE inhibitors or ARBs. It’s more effective at reducing hospitalizations and death. The number needed to treat to save one life over three years is just 12.
- Heart failure beta-blockers: Carvedilol, metoprolol succinate, or bisoprolol. These aren’t your regular blood pressure pills. They’re specifically chosen to slow heart damage.
- Mineralocorticoid receptor antagonists (MRAs): Spironolactone or eplerenone. These reduce fluid buildup and scarring in the heart.
- SGLT2 inhibitors: Dapagliflozin or empagliflozin. Originally diabetes drugs, they now work for heart failure-even if you don’t have diabetes. They cut hospitalizations by nearly 25%.
These aren’t optional add-ons. They’re the foundation. And they work best when taken together, at full doses. But here’s the hard truth: only about 39% of eligible patients get all four within a year of diagnosis. Why? Many doctors are still hesitant. They worry about low blood pressure, kidney changes, or too many pills. But real-world data shows severe low blood pressure affects less than 2% of patients. The fear is bigger than the risk.
HFpEF: The Disease That Had No Treatment-Until Now
For years, HFpEF was the forgotten cousin of heart failure. Doctors could only prescribe diuretics to reduce swelling. No drug had proven it could save lives or keep you out of the hospital. That changed in 2021 with the EMPEROR-PRESERVED trial. Empagliflozin, an SGLT2 inhibitor, cut the risk of hospitalization or death from heart failure by 21%. The DELIVER trial with dapagliflozin showed similar results. By 2023, these drugs got a Class I recommendation-meaning they’re now standard care for HFpEF.
One patient in Sydney, 72, with HFpEF and type 2 diabetes, started empagliflozin after three hospitalizations in two years. Within three months, her 6-minute walk distance went from 320 meters to 410. She hasn’t been back to the hospital since. That’s not luck. That’s science.
But the benefit isn’t huge for everyone. The absolute reduction in risk over two years is about 1.6%. That means you need to treat 62 people to prevent one hospitalization. So it’s not for everyone-but for those with symptoms, it’s a game-changer.
Technology That Watches Your Heart From Inside
Some patients get a tiny sensor implanted in the pulmonary artery-the CardioMEMS HF System. It measures pressure in your lungs every day. If pressure starts rising, it means fluid is building up before you feel it. Your doctor gets the alert and can adjust your meds before you’re rushed to the ER.
Studies show this cuts hospitalizations by up to 37%. In the 2025 MONITOR-HF trial, patients using CardioMEMS had 28% fewer heart failure admissions and reported better quality of life. Medicare covers it for patients with repeated hospitalizations. But it’s not for everyone-it’s for those who keep bouncing back to the hospital despite meds.
One patient in Melbourne, 68, with Stage D HFpEF, had been hospitalized six times in 18 months. After getting CardioMEMS, he had zero admissions in the next year. His wife said, “It’s like having a nurse inside his chest.”
Why So Many People Still Fall Through the Cracks
Even with all these advances, care is uneven. A 2025 AHA report found Black patients are 37% less likely to get guideline-directed therapy than White patients-even after adjusting for income, education, and access. That’s not just a gap. It’s a crisis.
Another problem? Polypharmacy. The average HFrEF patient takes 7.3 medications daily. Add in pills for diabetes, arthritis, or depression, and it’s easy to miss a dose. One caregiver on HeartFailureMatters.org said, “My husband takes eight heart meds plus others. He forgets half the time.”
Tools like the ACC’s “HF in a Box” toolkit help. It includes checklists, patient education sheets in 17 languages, and simple dosing schedules. Clinics using it saw a 27% jump in patients getting full quadruple therapy within six months.

What You Can Do Right Now
If you’ve been diagnosed with heart failure, ask these questions:
- What’s my ejection fraction? Is it HFrEF, HFpEF, or something in between?
- Am I on all four recommended meds for HFrEF-or the right ones for HFpEF?
- Have we talked about CardioMEMS if I’ve been hospitalized more than once?
- Do I have a care plan that includes diet, activity, and a way to track weight daily?
Don’t assume your doctor knows everything. The latest guidelines are new. Many haven’t fully updated their practice. Bring printed summaries from the American Heart Association or the Heart Failure Society of America. Ask for the “HF in a Box” resources. You have the right to the best care available.
The Future Is Personalized
Researchers are now looking at why some patients respond better than others. One emerging area is CHIP-Clonal Hematopoiesis of Indeterminate Potential. It’s a genetic change in blood cells that triggers inflammation and increases heart failure risk by more than double. In people over 70, it’s found in 15-20%. Trials are testing anti-inflammatory drugs like canakinumab to target it.
Another frontier? Personalized blood pressure targets. A 2025 meta-analysis found low blood pressure (<90 mmHg) is dangerous in HFpEF but not in HFrEF. That means one size doesn’t fit all. The TARGET-HF trial, enrolling 4,200 patients across 150 sites, is testing whether tailoring BP goals to your heart failure type improves outcomes. Results are expected in 2027.
For now, the message is clear: heart failure is no longer a death sentence. With the right diagnosis, the right meds, and the right support, many people live years longer-and better-than ever before.
Can you reverse heart failure?
Reversal isn’t common, but improvement is. In HFrEF, patients on full quadruple therapy can see their ejection fraction rise by 10-15 points over 6-12 months. Some even move from severe to mild dysfunction. This is called “reverse remodeling.” It’s not a cure, but it means fewer symptoms, less hospitalization, and better survival. HFpEF doesn’t usually show this kind of structural improvement, but symptoms and quality of life can improve dramatically with SGLT2 inhibitors and lifestyle changes.
Do I need to stop all my other medications?
No. In fact, many heart failure patients need more meds-not fewer. But some may need adjustments. For example, if you’re on a diuretic for swelling, your doctor may reduce it once you start SGLT2 inhibitors, because those drugs also help remove fluid. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can worsen heart failure and should be avoided. Always check with your doctor before starting or stopping any medication, even over-the-counter ones.
Is it safe to exercise with heart failure?
Yes-when done safely. Regular, moderate exercise improves strength, reduces fatigue, and lowers hospitalization risk. Start with walking 10-15 minutes a day, five days a week. Use a heart rate monitor if you have one. Avoid heavy lifting or holding your breath. Cardiac rehab programs are ideal-they’re supervised, tailored, and proven to extend life. Even patients with advanced heart failure can benefit from light activity like seated exercises or stretching.
How much salt should I eat?
Limit sodium to less than 2,000 mg per day. That’s about one teaspoon of salt. But it’s not just the salt shaker. Processed foods, canned soups, bread, and restaurant meals are the biggest sources. Read labels. Choose fresh or frozen vegetables, plain meats, and whole grains. A low-sodium diet helps reduce fluid retention and lowers blood pressure. Many patients report feeling less bloated and more energetic after cutting back.
What if I can’t afford my heart failure meds?
Cost is a real barrier. SGLT2 inhibitors can cost over $500 a month without insurance. But most manufacturers offer patient assistance programs. For example, AstraZeneca’s Farxiga and Boehringer Ingelheim’s Jardiance have copay cards that can reduce monthly costs to under $10. Medicare Part D covers many heart failure drugs, and some states have additional aid programs. Talk to your pharmacist or social worker-they can help you find options. Never skip doses because of cost. There are solutions.
Next Steps: What to Do Today
If you’re newly diagnosed, schedule a follow-up with a heart failure specialist within 30 days. Ask for a medication review. Get a weight scale and check your weight every morning. Write down any new swelling, shortness of breath, or dizziness. Bring this log to your next visit.
If you’ve had heart failure for years, ask if you’re on all four recommended drugs for HFrEF-or if SGLT2 inhibitors are right for you if you have HFpEF. Ask about CardioMEMS if you’ve been hospitalized more than once. Ask if you qualify for cardiac rehab.
Heart failure management today isn’t about waiting for the next crisis. It’s about building a daily routine that protects your heart. With the right care, you don’t just survive-you live.




November 22, 2025 AT 22:58 PM
Just read this and felt like crying. My dad’s been on all four meds for HFrEF since last year, and he’s walking the dog again without stopping. I used to think heart failure meant giving up - turns out it’s about fighting smarter. Thanks for laying this out so clearly. 🙏
November 23, 2025 AT 03:01 AM
Big Pharma pushed these drugs hard and now everyone’s acting like it’s magic. What about the side effects nobody talks about? Kidney damage? Low BP? They’re just selling pills not cures
November 23, 2025 AT 22:47 PM
You know in India we say ‘dard ka ilaj nahi, dard ke saath rehna seekho’ - learn to live with the pain. But here? We’re trying to erase the pain with pills and implants. Is that healing or just delaying the inevitable? The heart doesn’t care about guidelines - it just beats, or it doesn’t.
November 25, 2025 AT 19:52 PM
The American Heart Association guidelines are not infallible. In fact, they have been repeatedly influenced by pharmaceutical lobbying. The so-called 'quadruple therapy' is a textbook example of guideline creep driven by profit margins, not patient outcomes. This is not medicine - it's corporate medicine.
November 25, 2025 AT 20:08 PM
I’ve seen too many elderly patients on 10+ medications, confused, falling, dying in nursing homes. This ‘quadruple therapy’ is just a recipe for polypharmacy chaos. Why not just let nature take its course? We’re medicalizing death now.
November 27, 2025 AT 02:56 AM
I work in cardiology and I’ve seen this happen. Doctors ignore HFpEF because they don’t know what to do. Then some drug company gives them a free lunch and suddenly everyone’s prescribing dapagliflozin like it’s aspirin. And no one checks if the patient can even swallow pills anymore.
November 27, 2025 AT 11:47 AM
In Nigeria we don’t even have ACE inhibitors in rural clinics. You talk about SGLT2 inhibitors like they’re candy. We’re lucky if we get furosemide. This whole article is a luxury for the West. Meanwhile, our people die from hypertension because they can’t afford to check their BP. #GlobalHealthInjustice
November 29, 2025 AT 02:51 AM
Interesting that CHIP is mentioned. Recent data from the UK Biobank suggests CHIP carriers with HFrEF have higher inflammatory markers and respond poorly to standard therapy. Could anti-inflammatories be the next tier? Also - has anyone looked at gut microbiome changes in HFpEF? Emerging links there.
November 29, 2025 AT 13:11 PM
Look, I get it - we’re all excited about new drugs, new tech, new guidelines. But let’s be real: 80% of these patients are over 70. They’re not ‘living well’ - they’re surviving on a cocktail of pills, with their kidneys screaming, their blood pressure crashing, and their families exhausted. The system is optimized for metrics, not meaning. The real question isn’t ‘can we treat it?’ - it’s ‘should we?’ And who decides? The cardiologist? The insurer? The FDA? Or the patient who just wants to sit on the porch without feeling like they’re drowning?
And don’t get me started on CardioMEMS. $30,000 for a sensor that alerts doctors before you get sick? That’s not healthcare. That’s insurance fraud with a tech veneer. Who pays for it when Medicare says ‘no’? The patient? The family? The hospital? It’s a beautiful gadget for a broken system.
I’ve sat with people who’ve had three hospitalizations in a year. They don’t care about EF percentages. They care about breathing without a pillow. They care about not being a burden. They care about tasting coffee again without gasping. We’ve turned heart failure into a technical problem to be solved - but it’s a human one. And we’re failing at that.
And yet - somehow - we keep pretending that more pills, more sensors, more guidelines = better care. We’re not healing people. We’re managing decline with algorithms.
December 1, 2025 AT 11:59 AM
My mom had HFpEF and got on dapagliflozin. She lost 12 pounds in a month. Didn’t even realize she was bloated until she could tie her shoes again. I’m not a doctor but I know what I saw. This stuff works.
December 1, 2025 AT 13:29 PM
They say SGLT2 inhibitors help HFpEF... but what if it’s just because they make you pee more? Like... is it really fixing the heart or just flushing out the fluid? And who funded those trials again? I smell a rat.
December 1, 2025 AT 17:56 PM
And yet, the same companies that pushed SGLT2 inhibitors for heart failure also spent $200M lobbying to block Medicare from negotiating drug prices. You think they care about your aunt’s quality of life? They care about the next quarterly report. This isn’t medicine - it’s capitalism with a stethoscope.
Meanwhile, Black patients are still 37% less likely to get these drugs. So who’s really benefiting? The ones who can afford to ask the right questions. The rest? They’re just data points in a clinical trial.
December 2, 2025 AT 19:12 PM
I love how we treat heart failure like a software update - just install the new patches and you’re good. But the heart isn’t a phone. It’s a living organ that’s been fighting for decades. Maybe we should spend less time optimizing drugs and more time teaching people how to breathe, how to rest, how to live with limits.
December 4, 2025 AT 07:28 AM
Let’s be honest - if this was a cancer drug with this kind of data, we’d be holding parades. But because it’s heart failure - and because it affects old people - we treat it like a nuisance. We don’t fund research like we do for melanoma. We don’t make memes about SGLT2 inhibitors. We don’t celebrate survivors. We just say ‘well, he’s 78, what did you expect?’
That’s the real disease here. Not the failing heart. The apathy.
December 5, 2025 AT 09:07 AM
I’ve been caring for my husband with Stage C HFrEF for 3 years. We use the HF in a Box checklist. It changed everything. I printed it, laminated it, stuck it on the fridge. Now I know what to ask. I don’t feel so lost anymore.