Learn how to teach your family to recognize overdose signs like unresponsiveness, slow breathing, and skin color changes. Includes step-by-step training methods, naloxone use, and real-life survival tips.
Family Overdose Response: What to Do When Someone Overdoses
When a family member overdoses, every second counts. A family overdose response, the immediate actions taken by loved ones when someone shows signs of a drug overdose. Also known as household emergency protocol, it’s not about waiting for paramedics—it’s about acting before it’s too late. Most overdoses happen at home, often with no one else around. That means the person closest to them—their parent, partner, or child—is the first and most important responder.
You don’t need medical training to save a life. The key tools are awareness, naloxone, and a calm head. Naloxone, a medication that reverses opioid overdoses by blocking opioid receptors in the brain. Also known as Narcan, it’s safe, easy to use, and works in minutes. Keep it in your medicine cabinet, your car, your purse. It’s not just for heroin or fentanyl—it works on any opioid, including prescription painkillers. And if you’re unsure whether someone overdosed, give it anyway. It won’t hurt someone who didn’t take opioids.
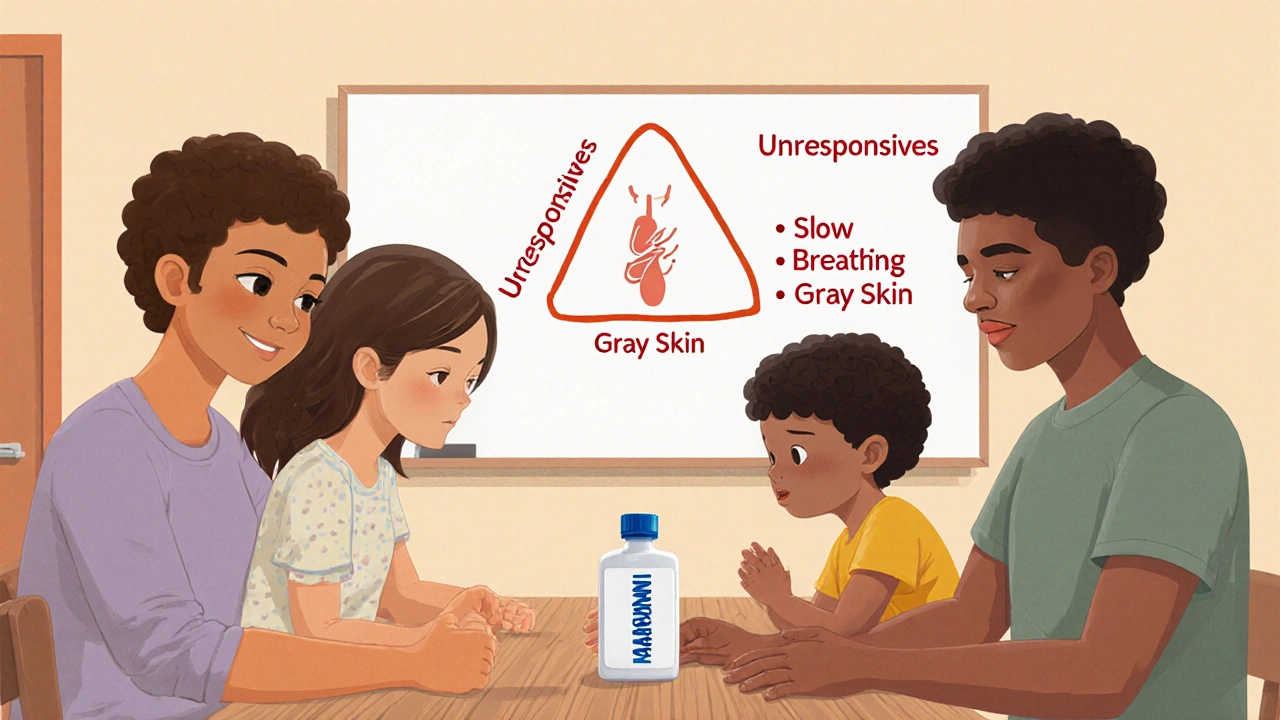
But naloxone isn’t the whole story. You also need to know the signs: blue lips, slow or stopped breathing, unresponsiveness, gurgling sounds. Don’t wait for all of them. If someone’s not waking up and isn’t breathing normally, start CPR and call 911. Opioid overdose, a life-threatening condition caused by too much opioid in the body, leading to respiratory failure. Also known as respiratory arrest from opioids, it kills quietly—no screams, no drama. Many families think overdoses only happen to strangers or "addicts." They don’t realize it can happen to their teenager after a sports injury, their parent after years of pain meds, or their sibling after a relapse. That’s why education isn’t optional—it’s survival.
There’s no shame in preparing. Keep naloxone. Learn how to do chest compressions. Talk to your family about what to do if someone stops breathing. Practice with a training kit. Most pharmacies give naloxone without a prescription, and many community centers offer free training. This isn’t about judgment—it’s about love. The people who need help the most are often the ones you care about the most.
In the posts below, you’ll find real, practical guides on how to recognize an overdose, how to use naloxone correctly, what to say to emergency responders, and how to prevent future incidents. You’ll also learn about the hidden risks of mixing medications, why some overdoses are harder to reverse, and how to talk to your doctor about keeping naloxone at home. This isn’t theory. These are the steps that have saved lives in real homes, with real families. You don’t need to be an expert. You just need to be ready.