Explore how chronic hepatitis B raises heart disease risk, the science behind it, and practical steps to protect your cardiovascular health.
Cardiovascular Risk: What It Is and How to Manage It
When working with cardiovascular risk, the probability of developing heart disease or stroke based on lifestyle, genetics, and existing health conditions. Also known as heart risk, it helps doctors and patients decide which prevention steps to take. Think of it as a scoreboard that adds points for each unhealthy factor you have. The higher the score, the more likely you’ll face a cardiac event. In this guide we’ll break down the biggest score‑boosters, show how they interact, and point you toward practical ways to lower the total.
Key Factors That Drive Cardiovascular Risk
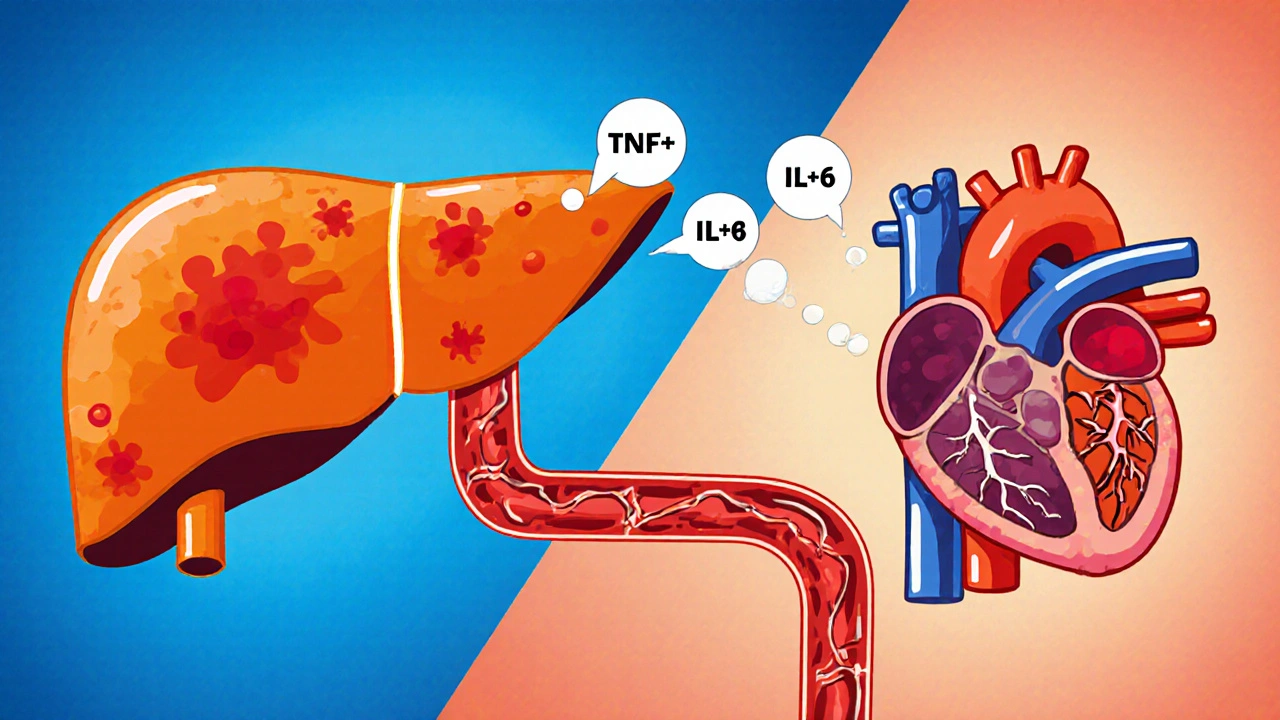
One of the top contributors is blood pressure, the force exerted by circulating blood against artery walls. When it stays high, arteries stiffen and plaque builds faster. Another major player is cholesterol, the waxy substance that can clog arteries if LDL levels rise. Elevated LDL is like oil spilling into a pipe—you get blockages that lead to heart attacks. Diabetes, a condition where blood sugar regulation is impaired, also piles on extra points; high glucose damages blood vessels and speeds up plaque formation. Add smoking, a habit that inflames lining, and you’ve got a perfect storm for cardiovascular risk.
These factors don’t act alone. For example, high blood pressure often co‑exists with high cholesterol, and the combination multiplies danger more than the sum of each part. That’s why clinicians look at the whole picture, not just one number. In fact, the relationship can be expressed as a simple triple: cardiovascular risk encompasses blood pressure levels, high cholesterol contributes to cardiovascular risk, and diabetes increases cardiovascular risk. Understanding these links makes it easier to pick the right interventions.
So how do you measure your own score? The basics are a routine blood pressure check, a lipid panel for cholesterol, and a fasting glucose or HbA1c test for diabetes. Many online calculators let you plug these numbers in, along with age, sex, and smoking status, to get an estimated 10‑year risk. While calculators are handy, they’re only as good as the data you feed them. Keep records, repeat tests, and discuss trends with your doctor.
Once you know where you stand, the next step is action. Lifestyle changes—cutting back on salt, eating more vegetables, exercising regularly, and quitting smoking—can shave dozens of points off your risk score. If lifestyle alone isn’t enough, medications step in. For high blood pressure, beta‑blockers like propranolol or newer agents such as ACE inhibitors can tame the pressure. Elevated cholesterol often calls for statins; the cheap generic Lipitor (atorvastatin) is a common choice. When diabetes raises the risk, metformin helps control glucose and also has modest heart‑protective effects. Some newer drugs, like trimetazidine (Vastarel), target heart muscle efficiency directly, offering another layer of protection for high‑risk patients.
All of these options appear across the articles on this page. You’ll find side‑by‑side comparisons of propranolol versus other blood‑pressure meds, deep dives into how metformin stacks up against newer diabetes treatments, and a close look at anti‑ischemic agents like Vastarel. Together they form a toolbox you can use to lower your cardiovascular risk, whether you’re starting from scratch or fine‑tuning an existing regimen.
Ready to see the details? Below you’ll discover practical guides, drug comparisons, and lifestyle tips that help you turn the abstract idea of cardiovascular risk into concrete steps you can take today.
A detailed side‑by‑side look at ezetimibe versus statins, PCSK9 inhibitors, bile‑acid sequestrants, niacin, and lifestyle changes, covering efficacy, safety, cost, and how to pick the right cholesterol‑lowering therapy.