Chronic Hepatitis B Cardiovascular Risk Calculator
This tool estimates your cardiovascular risk based on your hepatitis B status and key health indicators. The calculator uses data from studies showing that chronic hepatitis B increases heart disease risk by approximately 30-40% compared to the general population.
Your Estimated Cardiovascular Risk
When discussing chronic hepatitis B is a long‑term infection of the liver caused by the hepatitis B virus (HBV), most people think only about liver cirrhosis or liver cancer. Yet a growing body of evidence shows that the virus also nudges the heart into trouble. This article walks through why the connection matters, how the risk builds, and what you can do today to protect your cardiovascular health.
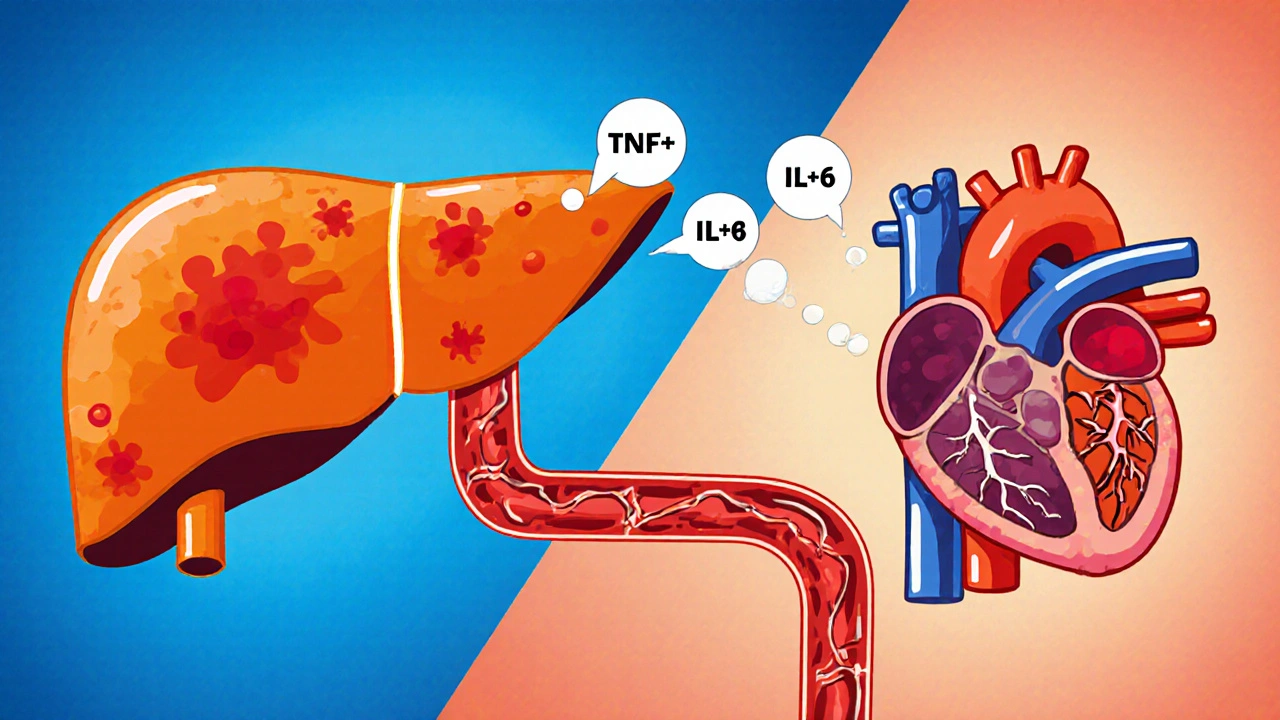
Why the Liver and Heart Talk to Each Other
The liver and heart share a two‑way street of chemicals, hormones, and immune signals. When the liver is inflamed, it releases cytokines such as tumor necrosis factor‑α (TNF‑α) and interleukin‑6 (IL‑6). Those molecules travel through the bloodstream and can damage blood‑vessel walls, a process known as endothelial dysfunction. Over time, this dysfunction seeds atherosclerosis, the main driver of heart disease.
Key Research Findings (2020‑2025)
Several large cohort studies from Asia, Europe, and North America have quantified the link:
- A 2022 meta‑analysis of 15 prospective studies (over 1.2 million participants) reported a pooled hazard ratio of 1.38 for cardiovascular events in people with chronic hepatitis B compared to those without infection.
- The Taiwan National Health Insurance database showed that patients with HBV DNA levels above 2,000 IU/mL had a 22 % higher risk of myocardial infarction over a 10‑year follow‑up.
- In a 2024 liver‑cardio cross‑sectional study, elevated ALT (alanine aminotransferase) levels correlated with increased arterial stiffness, measured by pulse wave velocity.
These numbers are not academic footnotes; they translate into real‑world outcomes-more heart attacks, more strokes, and higher cardiovascular mortality among chronic hepatitis B carriers.
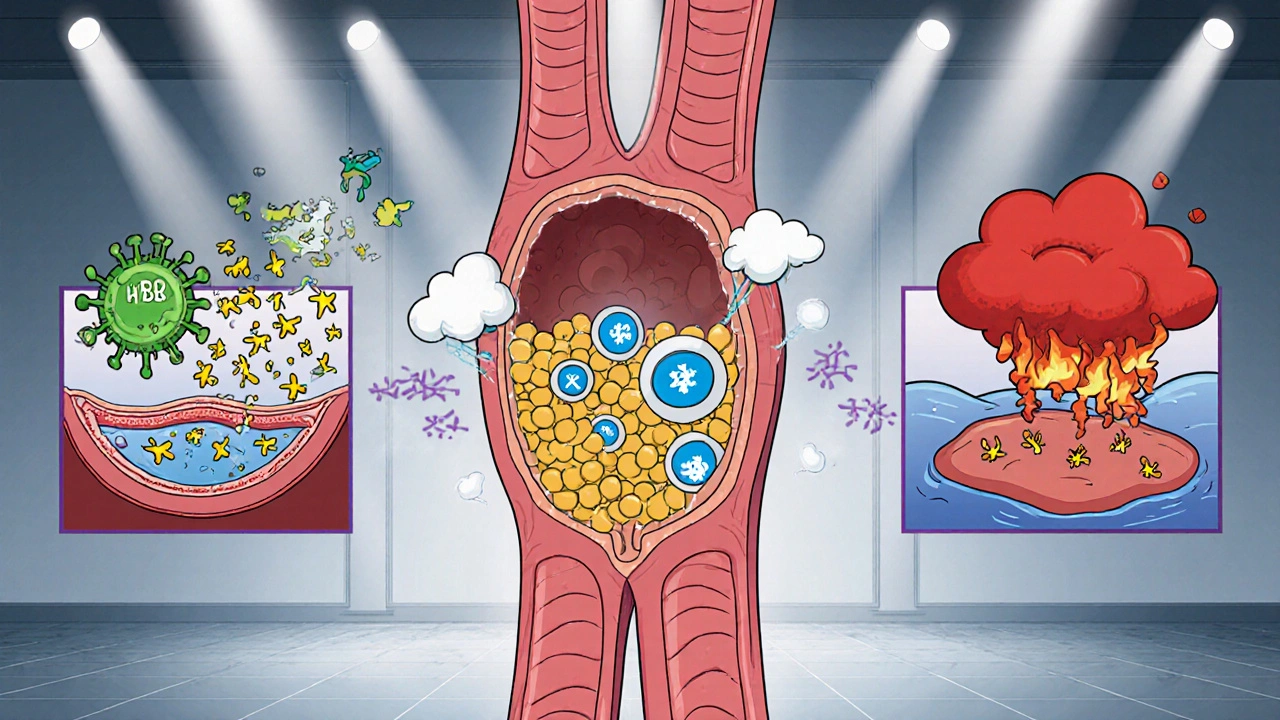
How the Virus Fuels Cardiovascular Risk
The mechanisms can be grouped into three overlapping pathways:
- Chronic systemic inflammation: Persistent viral replication keeps the immune system on high alert, flooding the blood with pro‑inflammatory cytokines that accelerate plaque formation.
- Metabolic disturbances: HBV infection can alter lipid metabolism, leading to higher low‑density lipoprotein (LDL) and lower high‑density lipoprotein (HDL) levels-both classic risk factors for atherosclerosis.
- Direct viral effects on vascular cells: Emerging lab data suggest HBV may infect endothelial cells, disrupting nitric‑oxide production and promoting clot formation.
Understanding these pathways helps clinicians target the right interventions, whether it’s antiviral therapy, statins, or lifestyle tweaks.
Antiviral Therapy: Does It Lower Heart Risk?
Modern nucleos(t)ide analogues-tenofovir disoproxil fumarate (TDF) and entecavir-suppress HBV DNA to undetectable levels in >95 % of patients. Several observational studies suggest that successful viral suppression reduces the inflammatory burden and, consequently, cardiovascular events.
Key points from recent data:
- Patients achieving undetectable HBV DNA had a 15 % lower incidence of coronary artery disease over five years.
- Long‑term TDF use was associated with modest improvements in lipid profiles (lower triglycerides, higher HDL).
- Switching from older agents like lamivudine to tenofovir further cut the risk of stroke by ~10 %.
While antiviral therapy is not a guarantee against heart disease, it is a strong piece of the prevention puzzle.
Practical Steps to Guard Your Heart
If you live with chronic hepatitis B, consider the following checklist. Each item tackles a specific risk driver discussed above.
- Know your viral load: Ask your doctor for the latest HBV DNA result. If it’s high, discuss initiating or optimizing antiviral therapy.
- Track liver enzymes: Elevated ALT often mirrors systemic inflammation. Aim for levels within the normal range (< 40 U/L for most labs).
- Screen for cardiovascular risk every 2-3 years: Include a lipid panel, fasting glucose, and blood pressure check.
- If LDL > 130 mg/dL, talk about statin therapy-even if you have normal liver enzymes, statins are safe in most HBV patients.
- Adopt a heart‑friendly diet: Emphasize omega‑3 fatty acids (fatty fish, walnuts), fiber‑rich vegetables, and limit processed sugars. This helps both liver and artery health.
- Stay active: Aim for at least 150 minutes of moderate‑intensity aerobic exercise weekly. Exercise lowers inflammatory markers and improves insulin sensitivity.
- Quit smoking and limit alcohol: Both substances worsen liver inflammation and accelerate atherosclerosis.
- Vaccinate against hepatitis A: Co‑infection can push liver inflammation higher, indirectly raising heart risk.
Following this list doesn’t replace regular medical care, but it gives you concrete actions you can start today.
Comparing Cardiovascular Risk: Chronic Hepatitis B vs General Population
| Risk Factor | General Population | Chronic Hepatitis B |
|---|---|---|
| Average HBV DNA (IU/mL) | Undetectable | Often >2,000 (if untreated) |
| ALT (U/L) | 30‑40 | 45‑120 (common elevation) |
| LDL (mg/dL) | 100‑130 | 115‑150 (slightly higher) |
| CRP (mg/L) - inflammation marker | 0.5‑2.0 | 2.5‑5.0 (elevated) |
| 5‑year cardiovascular event rate | ~4 % | ~5.5‑6 % |
The table highlights that, even after adjusting for age and gender, chronic hepatitis B nudges several numbers upward-especially inflammatory markers and LDL cholesterol. Those shifts translate into a modest but meaningful rise in heart‑related events.
When to Seek Specialist Care
Not every patient with hepatitis B needs a cardiology referral. However, consider a joint liver‑cardio consult if any of these flags appear:
- HBV DNA stays high (> 2,000 IU/mL) despite antiviral therapy.
- Persistent ALT elevation > 2× upper limit of normal.
- New onset hypertension, diabetes, or dyslipidemia.
- Family history of premature coronary artery disease.
A coordinated approach lets the hepatologist and cardiologist align treatment plans, possibly adjusting antiviral regimens or adding cardio‑protective drugs.
Future Directions: What Researchers Are Exploring
The link is still unfolding. Current trials are probing:
- The impact of adding PCSK9 inhibitors to HBV patients with stubborn LDL elevation.
- Whether novel anti‑inflammatory agents (e.g., IL‑1 blockers) can break the cycle of liver‑driven vascular inflammation.
- Genetic studies that may identify HBV‑specific polymorphisms predisposing to atherosclerosis.
Results could reshape guidelines within the next few years, making cardiovascular screening a routine part of hepatitis B management.
Quick Takeaways
- Chronic hepatitis B raises heart disease risk by roughly 30‑40 % across diverse populations.
- Systemic inflammation, altered lipids, and possible direct viral effects drive the link.
- Effective antiviral therapy, regular cardiovascular screening, and lifestyle changes markedly lower the added risk.
Does having chronic hepatitis B mean I will definitely get heart disease?
No. The virus raises the probability, but many patients never develop cardiovascular problems, especially if they control viral load, adopt a heart‑healthy lifestyle, and manage traditional risk factors.
Can I take statins if I have liver disease from hepatitis B?
Yes, in most cases. Modern statins are safe for patients with stable chronic hepatitis B. Your doctor will monitor liver enzymes before and after starting therapy.
How often should I get cardiovascular check‑ups?
If you’ve been diagnosed with chronic hepatitis B, aim for a full lipid panel, blood pressure reading, and fasting glucose every 2-3 years. Increase frequency if you have additional risk factors like smoking or diabetes.
Will antiviral medication lower my cholesterol?
Indirectly, yes. By suppressing HBV replication, antivirals reduce chronic inflammation, which can modestly improve lipid numbers. They don’t replace dedicated cholesterol‑lowering drugs when those are needed.
Is there a vaccine to protect my heart if I already have hepatitis B?
No vaccine targets the heart directly. The best protection is controlling the virus (antivirals) and following standard heart‑health measures-diet, exercise, and regular medical screening.


October 21, 2025 AT 20:26 PM
Living with chronic hepatitis B can feel overwhelming, especially when you hear about added heart risks. It helps to keep track of your viral load and stay on top of routine check‑ups.
November 11, 2025 AT 15:26 PM
Honestly the liver‑heart connection blew my mind but it makes sense once you think about all that inflammation floating around in the blood.
November 30, 2025 AT 03:52 AM
Yo, if you’re reading this and feel like the odds are stacked against you, remember you’ve got tools in your hands. First, get your HBV DNA tested; the numbers tell the story and guide treatment. Second, don’t ignore the power of lifestyle – a Mediterranean‑style diet rich in fish, nuts, and leafy greens cuts down on LDL and calms inflammation. Third, moving your body isn’t just for the muscles; steady cardio shaves off years of vascular wear and tear. Fourth, consider antiviral therapy if your doctor says you need it – suppressing the virus drops the cytokine storm and lets your arteries breathe. Fifth, keep your liver enzymes in the normal range; an ALT that’s too high is a red flag for systemic stress. Sixth, if your cholesterol is high, a statin is safe for most HBV patients and can further protect the heart. Seventh, quit smoking and limit alcohol; both are double‑whammy for liver and vessels. Eighth, schedule a lipid panel and blood pressure check every couple of years, or sooner if you have other risk factors. Ninth, get vaccinated against hepatitis A to avoid extra liver inflammation. Tenth, stay connected with a hepatologist and ask for a cardiology consult if you notice any new symptoms. Eleventh, keep a log of your meds and blood work so you can spot trends before they become problems. Twelfth, lean on support groups – sharing experiences makes the journey less lonely. Thirteenth, don’t let fear paralyze you; proactive steps can lower that 30‑40 % risk dramatically. Fourteenth, celebrate small wins – each normal test result is a victory. Fifteenth, remember that you’re not defined by a virus; you’re steering your own health ship, and the horizon looks bright when you combine treatment with heart‑smart habits.
December 17, 2025 AT 12:32 PM
From an ethical standpoint, it’s unforgivable to ignore the cardiovascular implications of a chronic infection. The medical community has a duty to flag these risks early and integrate liver‑cardio care.
January 2, 2026 AT 17:26 PM
Seriously, people act like they can just brush off the data – 22% higher heart attack risk isn’t a joke. If you’re still playing with your health, you deserve the consequences.
January 17, 2026 AT 18:32 PM
Take the meds, eat right, move daily – simple steps that add up to big protection.
January 31, 2026 AT 15:52 PM
Oh great, another post telling us to “just live healthier.” As if millions of HBV carriers don’t already know the basics.
February 13, 2026 AT 09:26 AM
Wow, the numbers really hit home – a tiny shift in LDL, a spike in CRP, and suddenly your heart’s in the crosshairs. It’s like a cinematic plot twist you didn’t see coming.