Statin Liver Risk Assessment Tool
Liver Enzyme Assessment
This tool provides evidence-based guidance on managing elevated liver enzymes while on statin therapy. Based on current medical guidelines, statin-related liver enzyme elevations are common but rarely dangerous.
Your results suggest that your elevated liver enzymes are likely not a significant concern. Based on current guidelines, you should not stop your statin therapy. Continue monitoring, retest in 4-6 weeks, and discuss with your doctor.
Note: Over 70% of mild elevations return to normal on their own. Stopping your statin increases your risk of heart attack or stroke by 3 times compared to continuing therapy.
Important Consideration
If your liver enzymes are elevated above 3x ULN and persist after retesting, or if you have symptoms, discuss stopping the statin with your doctor.
When you start taking a statin to lower your cholesterol, the last thing you want to hear is that your liver enzymes are up. It sounds scary. It sounds like your liver is damaged. But here’s the truth: statin-related liver enzyme elevations are almost never dangerous - and stopping your statin because of them might be riskier than keeping it.
What Actually Happens When Liver Enzymes Rise on Statins
Statins can cause a rise in two liver enzymes: ALT (alanine aminotransferase) and AST (aspartate aminotransferase). These enzymes leak into the blood when liver cells are stressed - not necessarily destroyed. In most cases, this is like a mild fever: a signal, not a crisis.
Only about 0.5% to 2% of people on statins see their ALT or AST rise above three times the upper limit of normal (3x ULN). That’s the clinical threshold. Even then, most of these people feel absolutely fine. No jaundice. No fatigue. No pain. Just a lab result that looks alarming on paper.
Studies tracking millions of statin users over decades show that serious liver injury - like liver failure - happens in fewer than 1 in 100,000 people per year. That’s rarer than being struck by lightning. The FDA reviewed 20 million patient-years of data and found only 32 confirmed cases of statin-induced acute liver failure between 1990 and 2020.
Why Do Some People See Enzyme Elevations?
It’s not random. There are patterns.
First, dose matters. Higher doses of statins - like 80 mg of atorvastatin or 40 mg of rosuvastatin - are more likely to cause a rise than low doses. Second, genetics play a role. A variant in the SLCO1B1 gene (the *521T>C variant) makes some people 3 times more likely to have elevated enzymes. This gene controls how statins move into liver cells. If it’s faulty, the drug builds up and stresses the liver.
Also, some statins are riskier than others. Cerivastatin (taken off the market in 2001) had the highest risk. Today, simvastatin and lovastatin - which are broken down by the CYP3A4 enzyme - carry a slightly higher risk, especially if you’re also taking antibiotics like clarithromycin or antifungals like ketoconazole. Pravastatin and rosuvastatin, which don’t rely heavily on CYP3A4, are the safest bets.
And here’s the twist: people with fatty liver disease (NAFLD) - the most common liver condition in the U.S. - actually have lower rates of statin-induced enzyme elevations than those with healthy livers. The reason? Statins may help reduce fat in the liver. They’re not hurting it; they might be healing it.
What Doctors Used to Do - and Why They Stopped
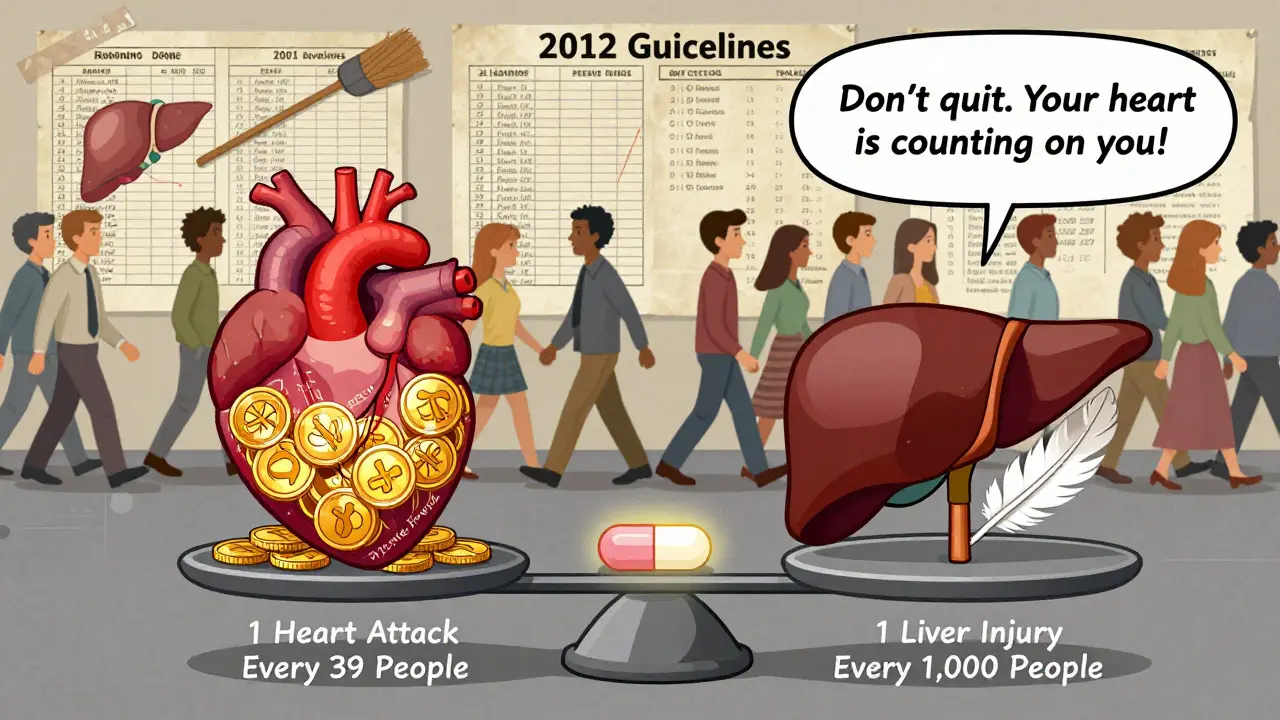
Back in 2001, guidelines said to check liver enzymes every 6 months on statins. That changed in 2012.
The FDA reviewed all the data and found something shocking: routine testing didn’t catch serious liver damage early. It didn’t prevent it. It just created anxiety, unnecessary follow-ups, and cost. A study in the Journal of the American College of Cardiology showed that 97% of enzyme elevations on statins were mild, temporary, and didn’t lead to liver injury.
Today, the American College of Cardiology, the American Heart Association, and the FDA all agree: check liver enzymes once before you start a statin. Then, only check again if you develop symptoms - like dark urine, yellowing skin, right-sided abdominal pain, or unexplained fatigue.
Yet, in 2023, over a third of U.S. primary care doctors still order routine tests. Why? Habit. Fear. Misinformation. This costs the healthcare system over $1.2 billion a year - all for tests that don’t change outcomes.
What to Do If Your Enzymes Go Up
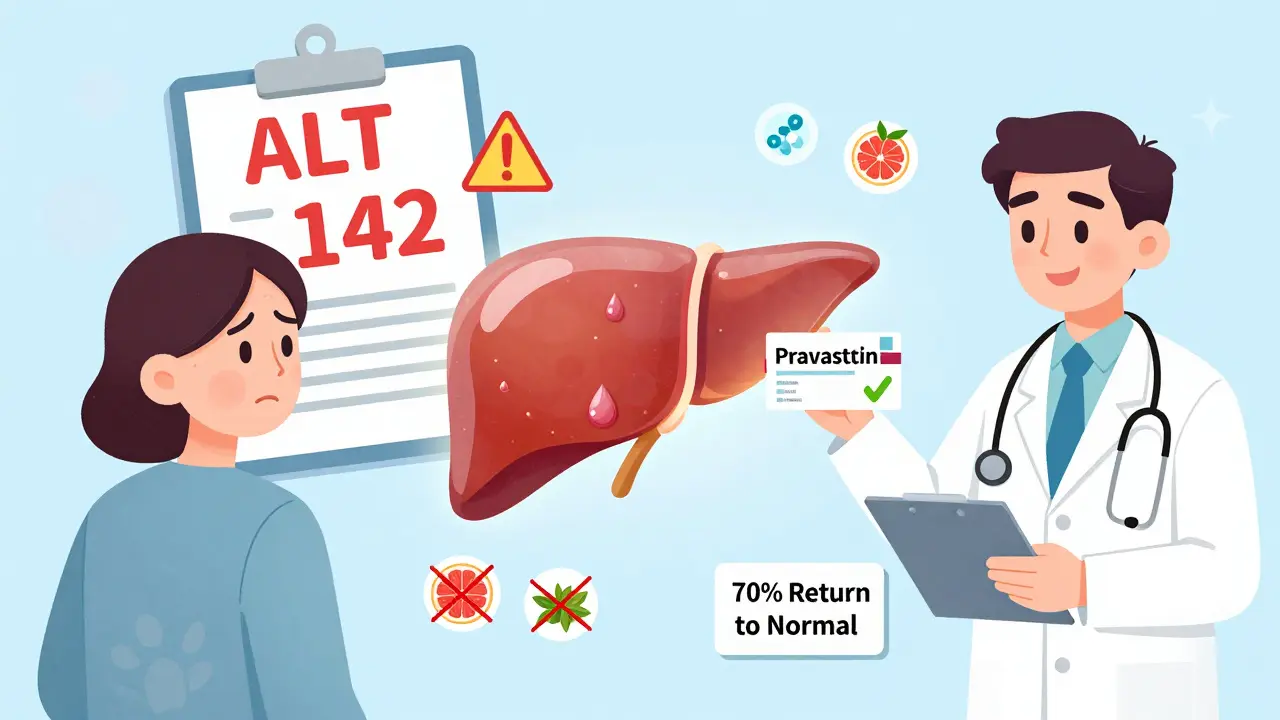
Let’s say your ALT is 142 U/L (2.5x ULN). You’re not sick. No symptoms. You’ve been on atorvastatin for 10 weeks. What now?
- Don’t panic. This is common. It’s not a sign of liver damage.
- Don’t stop the statin. Stopping increases your risk of heart attack or stroke. Studies show 5 out of 17 patients who quit statins over mild enzyme rises had a cardiac event within 18 months.
- Wait 4-6 weeks. Retest. In 70% of cases, the enzymes go back to normal on their own.
- If it’s still high, switch statins. Try pravastatin or rosuvastatin. Many patients see enzymes drop back to normal after the switch. One Reddit user saw his ALT fall from 142 to 38 after switching from atorvastatin to pravastatin.
- Rule out other causes. Viral hepatitis, alcohol, NAFLD, or even certain supplements (like green tea extract or high-dose niacin) can raise enzymes. Your doctor should test for these before blaming the statin.
Only if your enzymes go above 3x ULN and stay there after retesting - and you have symptoms - should you consider stopping the statin. And even then, rechallenge (trying it again later) is often safe.
Who’s at Higher Risk?
Not everyone is the same. Some people need extra caution:
- People over 75 with reduced kidney function (creatinine clearance under 30 mL/min) - their risk of enzyme rise is nearly 5 times higher.
- Those taking high-dose statins combined with CYP3A4 inhibitors (like clarithromycin, diltiazem, or grapefruit juice in large amounts).
- Patients with pre-existing liver disease (like cirrhosis) - though even here, moderate doses of rosuvastatin or atorvastatin are now considered safe under new European guidelines.
For everyone else? Statins are safer than most over-the-counter painkillers when it comes to liver risk.
The Bigger Picture: Why This Matters
Statin-related liver enzyme elevations are a classic case of a small, harmless signal being misinterpreted as a major threat.
Patients are terrified. A 2021 survey found that nearly 7 out of 10 statin users worry deeply about liver damage - even though only 1.2% ever see a true elevation above 3x ULN. That fear leads to real harm: 22% of statin users have stopped the drug at least once because of liver concerns. And many of them paid the price.
One study found that patients who stopped statins over mild enzyme elevations had 3 times the risk of heart attack or stroke in the next year. The number needed to treat to prevent one heart attack with statins is 39. The number needed to harm to cause one liver injury? 1,000.
That means for every 1,000 people on statins, one might get a mild enzyme rise. But for every 39 people on statins, one heart attack is prevented. The math is clear.
What’s New in 2025?
There’s progress on the horizon.
In 2023, the FDA approved a genetic test called StatinSafety Plus that checks for the SLCO1B1 and CYP3A4 variants. It’s 84% accurate at predicting who’s at risk. But it’s expensive - and only worth it for people on high-dose statins with existing liver issues.
Researchers are also testing coenzyme Q10 (CoQ10) supplements to protect the liver. In one trial, CoQ10 cut statin-induced enzyme elevations by 43%. But we don’t yet know if it helps prevent heart attacks - so it’s not recommended yet.
The European Society of Cardiology’s 2024 guidelines now say that even people with compensated cirrhosis (Child-Pugh A) can safely take moderate statin doses. This is a major shift. It means statins aren’t just tolerated by damaged livers - they may help them.
Bottom Line: Don’t Let a Lab Result Stop Your Statin
Statin-related liver enzyme elevations are common. They’re almost always harmless. They’re not a reason to stop your medication.
Stopping your statin because of a mildly elevated enzyme test is like stopping your seatbelt because you got a scratch on your shoulder. The real danger isn’t the scratch - it’s the crash you avoid by staying protected.
If your enzymes rise, talk to your doctor. Get retested. Rule out other causes. Consider switching statins. But don’t quit. Your heart is counting on you.
Can statins cause permanent liver damage?
No. Statins do not cause permanent liver damage. Even in rare cases where liver enzymes rise significantly, they almost always return to normal after stopping or switching the statin. There are no documented cases of permanent liver scarring or cirrhosis caused directly by statins in over 30 years of use.
Should I get my liver enzymes checked every 6 months on statins?
No. Major medical groups - including the FDA, American College of Cardiology, and American Heart Association - no longer recommend routine liver enzyme testing. Check once before starting, then only if you develop symptoms like jaundice, dark urine, or persistent nausea. Routine testing adds cost and anxiety without improving safety.
Is it safe to take statins if I have fatty liver disease?
Yes - and it may even help. People with nonalcoholic fatty liver disease (NAFLD) have a lower risk of statin-induced enzyme elevations than those with healthy livers. Statins can reduce liver fat and inflammation. Major guidelines now say NAFLD is not a reason to avoid statins.
Which statin is safest for the liver?
Pravastatin and rosuvastatin have the lowest risk of liver enzyme elevation. They are not metabolized by the CYP3A4 enzyme, which reduces interactions and liver stress. Simvastatin and lovastatin carry a slightly higher risk, especially at high doses or with certain medications.
What should I do if my liver enzymes are elevated but I feel fine?
Continue your statin, retest in 4-6 weeks, and ask your doctor to rule out other causes like alcohol, viral hepatitis, or supplements. Over 70% of mild elevations return to normal on their own. Stopping the statin increases your heart attack risk more than continuing it raises your liver risk.



February 14, 2026 AT 09:26 AM
Statins are the unsung heroes of heart health 😎 My ALT was 140 last year - panicked, retested in 6 weeks, back to normal. No drama. No stopping. Just keep chugging. Your liver ain’t mad, it’s just waving hello 👋
February 15, 2026 AT 12:32 PM
Man I used to freak out every time my doc mentioned liver enzymes. Then I read this whole thing and was like… wait, we’re scared of a lab number more than a heart attack? 😅 I switched from simva to prava and boom - enzymes dropped. No symptoms, no issues. Statins saved my life. Don’t let fear write your prescription.
February 16, 2026 AT 09:01 AM
Actually, you’re all missing the bigger picture. Did you know that the FDA’s data excludes non-Western populations? In India, we see way higher enzyme elevations - and it’s not just genetics. It’s the combination of statins + turmeric + chai + pollution. You’re generalizing based on skewed data. And yes, I’ve seen patients with ALT over 500 who didn’t even know they had fatty liver. So don’t be so quick to say it’s harmless.
February 17, 2026 AT 22:55 PM
So what you’re saying is… we should ignore all medical guidelines because some doctor is lazy? Classic. My cousin’s husband’s neighbor had liver failure after statins. You think that’s coincidence? Probably not. I’m not scared of heart attacks - I’m scared of being turned into a lab rat.
February 18, 2026 AT 06:13 AM
Let me get this straight - you’re telling me we should keep giving people potent CYP3A4 inhibitors while ignoring the fact that 97% of enzyme elevations are ‘harmless’? That’s not science. That’s corporate propaganda dressed up as a blog post. Also, who approved this? A pharma rep with a PowerPoint?
February 19, 2026 AT 01:02 AM
statins r bad. i read it on reddit. my buddy in lagos stopped and his cholestrol went down. also liver enzymes are a lie. they just want you to buy more pills. 1.2 billion? thats a lot of money. they dont care about you. they care about profit. #statinsareascam
February 20, 2026 AT 03:02 AM
I've been on statins for 12 years. My mom died of liver failure at 68. My aunt had a transplant. My cousin's boyfriend's cousin had a stroke after stopping statins. I'm not stopping. I'm not restarting. I'm not trusting anyone. I'm getting a second opinion. And a third. And a fourth. And I'm writing a letter to Congress. And I'm changing my diet. And I'm doing yoga. And I'm drinking celery juice. And I'm fasting. And I'm meditating. And I'm praying. And I'm crying. And I'm not alone.
February 20, 2026 AT 14:42 PM
Western medicine has failed us. In India, we treat liver health with turmeric, neem, and yoga. Why are we blindly trusting American guidelines? Statins are a colonial tool. They profit from fear. Our ancestors lived to 90 without statins. We must reclaim our health. This post is propaganda. I refuse to be a lab rat for Big Pharma.
February 22, 2026 AT 06:20 AM
This is one of the clearest, most reassuring pieces I’ve read on statins in years. Seriously - thank you. I’ve had patients quit statins over enzyme spikes and then end up in the ER with a heart attack. The fear is real, but the risk is backwards. Keep sharing this. We need more of this kind of calm, data-driven truth.
February 23, 2026 AT 12:34 PM
Love this. Simple. Clear. No fluff. Just facts. I’ve been telling my patients for years - if you feel fine and your enzymes are under 3x ULN, keep going. The real danger isn’t the liver - it’s the fear. And the cost. And the unnecessary tests. Keep fighting the noise.
February 25, 2026 AT 04:39 AM
While the data presented is compelling, it is imperative to acknowledge the limitations of retrospective cohort studies in capturing idiosyncratic adverse reactions. Additionally, the exclusion of non-Caucasian populations in many referenced trials may introduce selection bias. A nuanced, individualized approach remains paramount.
February 26, 2026 AT 21:13 PM
My doc ordered a liver test after 3 weeks on statins. I was like ‘uhhh no’ and kept going. Two months later, enzymes were down. I felt better than ever. Don’t let a number scare you. Your heart doesn’t care about your ALT. It just wants you to stay alive. 💪
February 27, 2026 AT 05:29 AM
Bro. I had ALT 150. I was SCARED. I googled ‘statin liver failure’ and watched 3 YouTube videos of people on deathbeds. Then I read this. Changed statins. Now my enzymes are normal. I’m alive. My heart is happy. 🤝🫡 Thanks for this. Someone should make a TikTok of this.
February 28, 2026 AT 07:21 AM
This is fascinating. I never realized statins might actually help fatty liver. I’ve been on one for 8 years, and my NAFLD diagnosis was just ‘watch and wait.’ Now I’m wondering if my liver’s been quietly thanking me. Also - the CoQ10 trial? That’s wild. I’m gonna ask my doc. Not because I’m scared - but because I’m curious. Knowledge is power, right?