Propranolol vs. Alternatives: Decision Helper
Patient Profile
Answer the following questions to get personalized recommendations.
Recommended Alternatives
When you or a loved one need a medication to lower blood pressure, control heart rhythm, or manage migraine attacks, the first name that pops up is often Propranolol is a non‑selective beta‑blocker that blocks both beta‑1 and beta‑2 receptors, reducing heart rate and contractility. It’s been on the market since the 1960s and is prescribed for hypertension, angina, arrhythmias, and even tremor. But you might wonder whether there’s a Propranolol alternatives that fits your lifestyle better, has fewer side effects, or offers once‑daily dosing.
Key Takeaways
- Propranolol is non‑selective; many newer beta‑blockers are cardio‑selective and cause fewer respiratory issues.
- Metoprolol and atenolol are the most common cardio‑selective substitutes, each with unique dosing schedules.
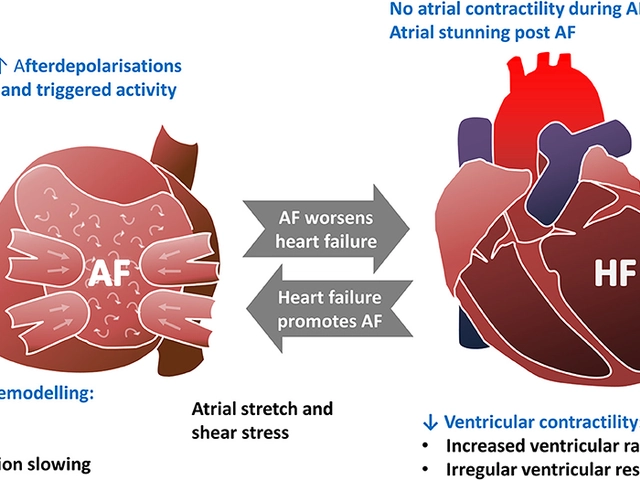
- Combination blockers like carvedilol and labetalol add alpha‑blocking activity, useful for specific heart‑failure cases.
- Calcium‑channel blockers (e.g., amlodipine) and ACE inhibitors (e.g., lisinopril) are not beta‑blockers but often serve as alternative first‑line options for hypertension.
- Choosing the right drug depends on age, comorbidities, lifestyle, and how your body reacts to side‑effects.
How Propranolol Works and When It’s Chosen
Propranolol binds to beta‑adrenergic receptors in the heart, lungs, and vascular smooth muscle. By preventing adrenaline and noradrenaline from activating these receptors, it slows the heart, lowers cardiac output, and reduces blood pressure. Clinicians favor it because it’s cheap, widely available, and effective for a broad range of conditions, including anxiety‑related tachycardia and migraine prophylaxis.
Decision Criteria for Selecting an Alternative
Before jumping to a different drug, ask yourself these questions:
- Do you have asthma or chronic obstructive pulmonary disease (COPD)? Non‑selective blockers can tighten airways.
- Is once‑daily dosing important for adherence?
- Are you pregnant, breastfeeding, or planning to become pregnant?
- Do you have diabetes? Some beta‑blockers mask low‑blood‑sugar symptoms.
- Are you already on a medication that interacts with beta‑blockers (e.g., certain antidepressants or anti‑arrhythmics)?
Answering these helps narrow the field to the few alternatives that truly match your health profile.
Comparison Table: Propranolol and Common Alternatives
| Drug | Selectivity | Typical Dose (mg) | Once‑Daily? | Notable Contra‑indications |
|---|---|---|---|---|
| Propranolol | Non‑selective (β1 & β2) | 40-160 | No | Asthma, severe bradycardia |
| Metoprolol | β1‑selective | 50-200 (extended‑release) | Yes (ER) | Severe heart block, hypotension |
| Atenolol | β1‑selective | 25-100 | Yes | Bronchospasm, severe liver disease |
| Carvedilol | β1/β2 + α1 blocker | 6.25-25 (twice daily) | No | Asthma, severe heart failure (initially) |
| Labetalol | β1/β2 + α1 blocker | 100-400 (IV or oral) | No | Asthma, severe liver disease |
| Bisoprolol | Highly β1‑selective | 5-10 | Yes | Severe bronchospasm, bradycardia |
| Amlodipine | Calcium‑channel blocker | 5-10 | Yes | Severe aortic stenosis |
| Lisinopril | ACE inhibitor | 10-40 | Yes | Pregnancy (first trimester), angioedema |
Deep Dive into the Top Alternatives
Below we explore each contender in more detail, focusing on how they differ from propranolol in mechanism, dosing convenience, and side‑effect profile.
Metoprolol
Metoprolol is a cardio‑selective β1 blocker, meaning it mainly affects the heart while sparing the lungs. That makes it a go‑to for patients with mild asthma who still need blood‑pressure control. The extended‑release (ER) formulation lets you take a single pill once a day, boosting adherence. Common side effects include fatigue, dizziness, and occasional cold hands.
Atenolol
Atenolol also targets β1 receptors but has limited ability to cross the blood‑brain barrier, so it often causes fewer sleep disturbances than propranolol. It’s dosed once daily, which many patients love. However, it’s cleared by the kidneys, so dose adjustments are needed for chronic kidney disease.
Carvedilol
Carvedilol combines β‑blocking with α1‑blocking, leading to vasodilation as well as heart‑rate reduction. This dual action is valuable in heart‑failure patients where after‑load reduction matters. The downside is a higher incidence of orthostatic hypotension, especially when starting therapy.
Labetalol
Labetalol works similarly to carvedilol but is often used in acute hypertension crises because it can be given intravenously. Oral labetalol’s twice‑daily schedule can be a hassle, and it shares the bronchospasm risk of non‑selective β‑blockers.
Bisoprolol
Bisoprolol is highly β1‑selective and is usually prescribed for chronic heart‑failure management. Its low dose range (5‑10mg) and once‑daily dosing make it convenient, yet patients with severe COPD still need caution.
Non‑Beta‑Blocker Alternatives
If beta‑blockers aren’t suitable, clinicians often turn to other classes. Amlodipine, a calcium‑channel blocker, relaxes arterial smooth muscle and is taken once daily. It’s gentle on the lungs but can cause ankle swelling. Lisinopril blocks the conversion of angiotensin I to II, lowering blood pressure and protecting kidneys - a solid choice for diabetic patients, though it’s contraindicated in early pregnancy.
Side‑Effect Profiles at a Glance
Understanding side‑effects helps you anticipate what might bother you and discuss alternatives with your doctor. Here’s a quick snapshot:
- Propranolol: fatigue, cold extremities, bronchospasm in asthmatics, can mask hypoglycemia.
- Metoprolol: dizziness, depression, reduced exercise tolerance.
- Atenolol: insomnia (rare), mild bradycardia, kidney‑dose adjustments.
- Carvedilol: orthostatic hypotension, weight gain (fluid retention).
- Labetalol: nausea, headache, potential for liver enzyme elevation.
- Bisoprolol: fatigue, occasional cough (less than non‑selective).
- Amlodipine: peripheral edema, flushing, gingival hyperplasia (rare).
- Lisinopril: dry cough, hyperkalemia, angioedema (rare).
Practical Tips for Switching or Starting Therapy
- Consult your prescriber before any change - abrupt withdrawal of propranolol can trigger rebound tachycardia.
- If moving to a cardio‑selective blocker, a typical conversion is propranolol 80mg → metoprolol 50mg (ER) or atenolol 50mg, but exact dosing should be individualized.
- Monitor blood pressure and heart rate for the first two weeks after a switch; keep a diary of any new symptoms.
- Consider timing: take beta‑blockers with food in the morning to avoid nighttime dizziness, unless the drug is specifically labeled for bedtime dosing.
- Check for drug interactions - beta‑blockers can enhance the action of insulin, digitalis, and some anti‑arrhythmic agents.

When to Stick With Propranolol
Even with many alternatives, propranolol remains the drug of choice for certain scenarios:
- Performance anxiety or situational tremor where its central nervous system penetration is beneficial.
- Migraine prophylaxis - propranolol’s ability to stabilize vascular tone outperforms many other agents.
- Cost‑sensitive settings - generic propranolol is often cheaper than newer branded beta‑blockers.
Bottom Line Decision Tree
Use this quick mental flowchart to decide:
- Do you have asthma or COPD? → Yes: Prefer cardio‑selective (metoprolol, atenolol, bisoprolol). No: Continue evaluating.
- Is once‑daily dosing crucial? → Yes: Metoprolol ER, atenolol, bisoprolol, amlodipine, lisinopril. No: Consider carvedilol or labetalol for heart‑failure needs.
- Do you need extra alpha‑blockade (e.g., heart‑failure with reduced ejection fraction)? → Yes: Carvedilol or labetalol.
- Are you pregnant or planning pregnancy? → Avoid ACE inhibitors in first trimester; beta‑blockers are category C-discuss risks.
Frequently Asked Questions
Can I replace propranolol with metoprolol for hypertension?
Yes, many doctors switch patients to metoprolol when lung issues are a concern. The typical conversion is 80mg of propranolol to about 50mg of metoprolol extended‑release, but the exact dose depends on your blood‑pressure targets and heart‑rate response.
Why does propranolol cause cold hands?
Blocking β2 receptors reduces vasodilation in peripheral vessels, so blood flow to the extremities drops, making hands feel cold. Cardio‑selective blockers spare β2 receptors and usually cause less peripheral cooling.
Is atenolol safe for people with kidney disease?
Atenolol is eliminated mainly by the kidneys, so dose reduction is required for moderate to severe renal impairment. Your doctor will calculate the appropriate dose based on your creatinine clearance.
Can I take propranolol and lisinopril together?
Yes, the two drugs work by different mechanisms and are often combined for better blood‑pressure control. Monitor for excessive drops in blood pressure and watch for signs of kidney function changes.
What are the signs of beta‑blocker withdrawal?
Sudden stopping can cause rebound tachycardia, hypertension, anxiety, and chest pain. Tapering over 1‑2 weeks under medical supervision minimizes these risks.
Is carvedilol better than propranolol for heart failure?
Clinical trials show carvedilol reduces mortality in systolic heart failure more effectively than non‑selective beta‑blockers like propranolol, mainly because its α1‑blocking adds vasodilation. However, it’s not the first choice for patients with asthma.
Next Steps
Take a piece of paper (or your phone) and answer the decision‑criteria questions above. Bring that list to your next doctor’s visit. If you’re already on propranolol and experience side effects, discuss a specific alternative-often a simple switch to a cardio‑selective blocker or a once‑daily formulation can make a huge difference in daily comfort.
Remember, no medication works the same for everyone. The goal is to find a safe, effective, and manageable drug that fits your life. Use the data here as a starting point, not a prescription.




October 5, 2025 AT 18:16 PM
Propranolol works, but if you have asthma consider cardio‑selective β‑blockers 😊.
October 9, 2025 AT 05:36 AM
Wow!!! This guide is incredibly thorough; I love how each alternative is broken down with clear pros and cons; truly a lifesaver!!!
October 12, 2025 AT 16:56 PM
i read the table and its super helpful but i still not sure which one fits me i think im leaning towards metoprolol
October 16, 2025 AT 04:16 AM
From a pharmacodynamic standpoint, the β1‑selectivity of metoprolol confers reduced bronchoconstrictive risk, making it optimal for patients with comorbid obstructive airway disease while preserving cardiac output modulation.
October 19, 2025 AT 15:36 PM
The decision matrix presented in this article meticulously juxtaposes the pharmacokinetic profiles of propranolol with its modern counterparts.
Each drug's selectivity, dosing frequency, and contraindication spectrum is enumerated with clinical precision.
Notably, the emphasis on cardio‑selective agents for asthmatic patients aligns with guideline‑driven practice.
The inclusion of bisoprolol as a highly β1‑selective option provides a valuable alternative for those seeking once‑daily dosing.
Moreover, the discussion of carvedilol’s α‑blocking properties elucidates its utility in systolic heart‑failure management.
The table also wisely lists non‑beta‑blocker classes such as amlodipine and lisinopril, reminding clinicians of first‑line options beyond adrenergic modulation.
The side‑effect synopsis, while succinct, captures the most clinically relevant adverse events, including bronchospasm and hypoglycemia masking.
For patients concerned with peripheral coldness, the contrast between non‑selective and β1‑selective agents is particularly instructive.
The practical tips for tapering propranolol underscore the risk of rebound tachycardia, a point often overlooked in outpatient settings.
The conversion examples, such as propranolol 80 mg to metoprolol ER 50 mg, offer a concrete starting point for dosage adjustments.
Importantly, the article flags the contraindication of ACE inhibitors during the first trimester, safeguarding maternal‑fetal health.
The nuanced discussion of renal clearance for atenolol highlights the necessity of dose modification in chronic kidney disease.
From a health‑economics perspective, propranolol’s low cost remains attractive for patients without comorbid respiratory concerns.
However, the adverse‑event profile may tip the balance toward a more selective β‑blocker in many scenarios.
Overall, the guide succeeds in translating complex pharmacological data into an accessible decision‑making tool for both clinicians and patients.
Clinicians are encouraged to individualize therapy based on the outlined criteria, ensuring optimal efficacy and tolerability.
October 23, 2025 AT 02:56 AM
In the grand theater of cardiovascular pharmacology, propranolol is the seasoned actor whose role has been rehearsed for decades, yet the understudies-metoprolol, atenolol, carvedilol-bring fresh nuance to the script of patient care.
October 26, 2025 AT 13:16 PM
Great summary! If you’re unsure which pathway fits your lifestyle, jot down the dosing schedule you prefer and bring that list to your appointment; it really streamlines the conversation.
October 30, 2025 AT 00:36 AM
Oh my gosh this article is like a rollercoaster of info!!! I was like totally lost at the table but then the side‑effect section hit me like a thunderbolt-soooo intense!!!
November 2, 2025 AT 11:56 AM
Nice overview, but the calcium‑channel blocker section feels tacked on.
November 5, 2025 AT 23:16 PM
For anyone transitioning from propranolol, start with a low dose of the chosen alternative and monitor both heart rate and any respiratory changes for at least a week; keep a log to discuss with your provider.
November 9, 2025 AT 10:36 AM
It is essential to recognize that abrupt discontinuation of propranolol can precipitate rebound hypertension; therefore, a supervised taper is advised to mitigate such risks.
November 12, 2025 AT 21:56 PM
Looks solid, though I’d add a note about drug‑interaction checks with antidepressants :)
November 16, 2025 AT 09:16 AM
While the exposition is commendably exhaustive, one might argue that the omission of nuanced beta‑blocker pharmacogenomics slightly diminishes the scholarly rigor of this treatise.
November 19, 2025 AT 20:36 PM
This guide is a waste of time; anyone with half a brain knows propranolol is outdated and should be tossed aside immediately.
November 23, 2025 AT 07:56 AM
Interesting read-metoprolol’s extended‑release formulation certainly offers convenience, yet the risk of orthostatic hypotension in the elderly should not be glossed over; consider starting at the lowest possible dose and titrating slowly.
November 26, 2025 AT 19:16 PM
One could contend that beta‑blockers, including propranolol, are overprescribed and that lifestyle interventions might outweigh pharmaceutical solutions in many mild hypertension cases.
November 30, 2025 AT 06:36 AM
Honestly, this is overly verbose; most clinicians just need the dosage conversion chart.
December 3, 2025 AT 17:56 PM
In the tapestry of patient care, each thread-be it a medication adjustment or a lifestyle habit-interweaves to create holistic wellness; thus, logging your vitals is not merely data collection but an act of self‑empowerment.
December 7, 2025 AT 05:16 AM
Sure thing but drug interactions are rare you dont need to stress about it
December 10, 2025 AT 16:36 PM
Stop romanticizing drugs; the reality is that propranolol can be life‑threatening for asthma patients and that’s a fact.