Living with diabetes means more than counting carbs or checking blood sugar. For nearly 7 out of 10 people with diabetes, nerve damage-called diabetic neuropathy-is a silent, painful reality. It starts subtly: a tingling in the toes, a burning sensation at night, or numbness that makes you trip on the rug you’ve walked on for years. Left unchecked, it can lead to foot ulcers, infections, and even amputations. But here’s the truth: pain from diabetic neuropathy doesn’t have to be your new normal. You can manage it. You can protect your nerves. And in some cases, you can even reverse the damage.
Why Your Nerves Are Hurting
Diabetic neuropathy isn’t caused by one thing-it’s the result of years of high blood sugar. Glucose sticks to proteins in your nerves like sticky syrup, messing up how signals travel. It also damages the tiny blood vessels that feed your nerves, starving them of oxygen and nutrients. The feet and legs take the biggest hit because those nerves are the longest. But over time, your hands and arms can get involved too. The damage isn’t always painful. Some people feel nothing at all-just numbness. That’s dangerous. If you can’t feel a blister forming on your heel, or a splinter stuck in your toe, it can turn into a serious infection. Others feel constant burning, stabbing, or electric shocks. This is called painful diabetic neuropathy (PDN), and it affects about 1 in 5 people with diabetes.Stop the Damage Before It Gets Worse
The single most powerful tool you have isn’t a pill. It’s your blood sugar. The Diabetes Control and Complications Trial proved it: keeping your HbA1c below 7% cuts your risk of nerve damage by 60%. That’s not a suggestion-it’s the foundation of everything else. What does that look like in real life?- Fasting blood sugar: 80-130 mg/dL
- After meals: under 180 mg/dL
- A1c: consistently below 7%
Pain Relief That Actually Works
If you’re already in pain, you need more than just better sugar control. You need targeted relief. And there are proven options. First-line medications are the most studied and recommended:- Duloxetine (Cymbalta): An antidepressant that also blocks pain signals. In clinical trials, 35% of patients had at least 50% pain reduction-twice the placebo rate.
- Pregabalin (Lyrica): An anticonvulsant that calms overactive nerves. Around 30-40% of users report major pain relief.
- Amitriptyline: An older tricyclic antidepressant. It works well-up to 60% pain reduction in some-but causes drowsiness, dry mouth, and weight gain. Not ideal for older adults.
- Capsaicin 8% patch (Qutenza): Applied once every 3 months in a doctor’s office. It depletes the pain chemical in nerve endings. 40% of users get 30%+ pain relief-with no drowsiness or stomach issues.
- Lidocaine patches (5%): Stick them right on the painful spot. Great for burning feet at night. Safe, cheap, and non-systemic.

When Pills Aren’t Enough
If medications fail, or side effects are too much, there are advanced options:- TENS units: Small devices that send gentle electrical pulses through your skin. In one study, 83% of users saw pain drop from 3.17 to 1.44 on a 5-point scale. No drugs. No needles. Just a battery-powered patch.
- Nerve blocks: A shot of numbing medicine near the affected nerve. Pain relief lasts weeks, sometimes months. Good for flare-ups.
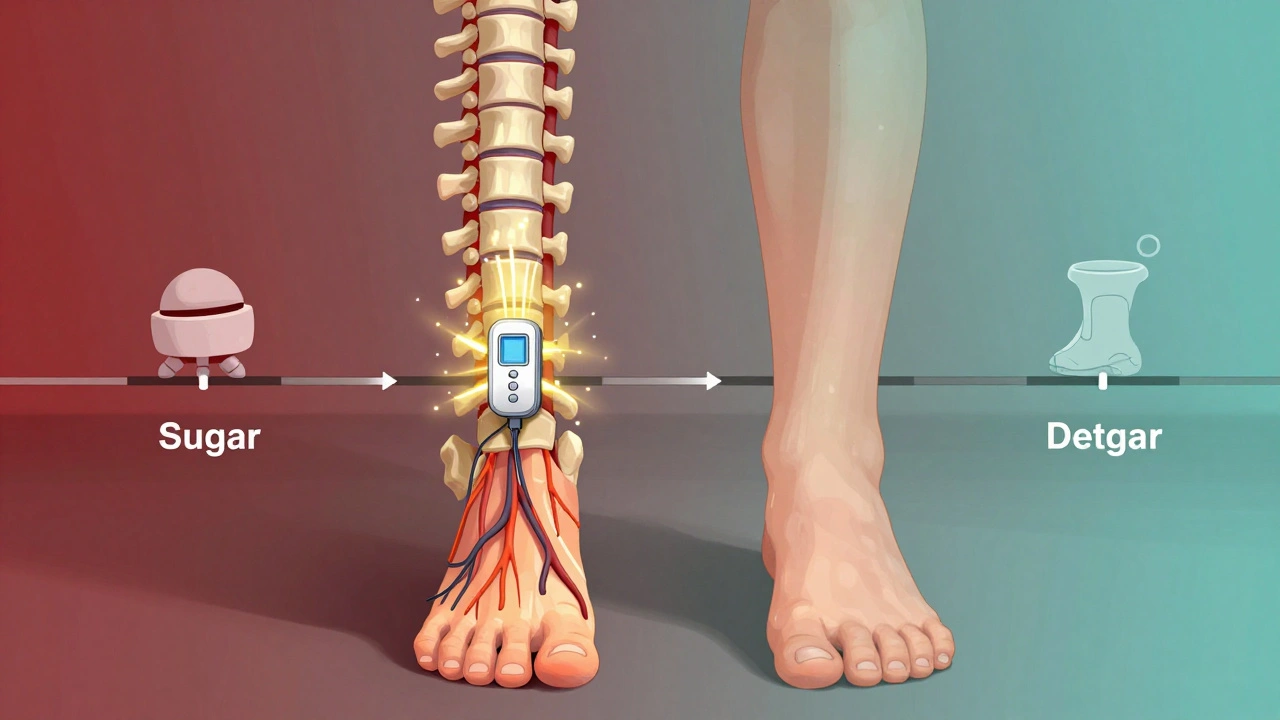
- Peripheral nerve stimulation: A tiny device is implanted under the skin near the painful nerve. It sends mild pulses to block pain signals. Works for 60-70% of people after 6 months.
- Spinal cord stimulation: This one’s groundbreaking. A device implanted near your spine doesn’t just dull pain-it can actually restore sensation. Patients report feeling their toes again after years of numbness. It’s not a cure, but it’s the closest thing we have to reversing damage.
Lifestyle: Your Secret Weapon
Medications treat symptoms. Lifestyle fixes the cause.- Move every day: Walking, swimming, cycling, yoga-anything that gets you moving for 30 minutes. Exercise improves blood flow to nerves and lowers blood sugar. Even if it hurts at first, keep going. Pain often improves within weeks.
- Eat to reduce inflammation: Focus on vegetables, fruits, beans, whole grains, fish, nuts, and lean proteins. Avoid sugary drinks, white bread, fried foods, and processed snacks. These spike blood sugar and fuel nerve damage.
- Check your feet daily: Use a mirror or ask someone to help. Look for cuts, blisters, redness, or swelling. Wash and dry them well-especially between the toes. Never go barefoot, even indoors.
- Manage stress: Chronic stress raises blood sugar and makes pain feel worse. Try deep breathing, meditation, or just 10 minutes of quiet every morning.
What Doesn’t Work-and What’s Coming
Tramadol and other opioids are sometimes prescribed. But they’re risky. The CDC says 8-12% of long-term users develop addiction. Nausea and constipation are common. They’re a last resort. As for future treatments? Researchers are testing drugs that target specific pain pathways in nerves. One targets Nav 1.7, a sodium channel that fires pain signals. Another blocks N-type calcium channels. There’s even a nerve growth factor antibody in trials. These aren’t available yet-but they’re the next frontier. The American Diabetes Association predicts that within 5-10 years, we’ll have therapies that don’t just mask pain, but actually repair damaged nerves. That’s not science fiction. It’s science in motion.What to Do Right Now
If you have diabetes and nerve pain:- Get your HbA1c tested. If it’s above 7%, work with your doctor to bring it down.
- Start checking your feet every day. No exceptions.
- Try a TENS unit or lidocaine patches-they’re safe and affordable.
- Ask your doctor about duloxetine or pregabalin if pain is keeping you up at night.
- Find a certified diabetes educator. They’ll help you build a real, sustainable plan-not just a list of meds.
Can diabetic neuropathy be reversed?
In mild cases, yes-especially if blood sugar is brought under control quickly. Nerve damage from short-term high glucose can improve within months. But if numbness or muscle weakness has been present for years, full reversal is unlikely. Still, many patients report reduced pain and even restored sensation with advanced treatments like spinal cord stimulation. The goal isn’t always complete recovery-it’s stopping further damage and improving quality of life.
Why does my neuropathy hurt more at night?
At night, your body isn’t distracted by movement or daily tasks. Pain signals become more noticeable. Also, cortisol levels-your body’s natural pain suppressor-drop during sleep. Plus, lying still can increase pressure on already sensitive nerves. Using a TENS unit, wearing soft socks, or applying a lidocaine patch before bed can help.
Is walking safe if my feet are numb?
Yes-but you must be careful. Wear well-fitting, cushioned shoes with no seams inside. Check your feet before and after walking for red spots or blisters. Use a mirror or ask someone to help inspect your soles. Walking improves circulation and helps lower blood sugar, which protects your nerves long-term. The risk of injury comes from not checking your feet, not from walking itself.
Can I use CBD oil for diabetic nerve pain?
There’s no strong clinical evidence yet that CBD oil reliably treats diabetic neuropathy. Some people report feeling better, but studies are small and inconsistent. It’s not FDA-approved for this use. If you’re considering it, talk to your doctor first-CBD can interact with other medications, including those for diabetes and blood pressure.
How long does it take for nerve pain to improve after better blood sugar control?
For some, pain starts easing within 3-6 months. Others take a year or more. The more severe the damage, the slower the improvement. But many patients report less burning, fewer nighttime awakenings, and improved balance after 12 months of consistent glucose control. Patience matters-but so does persistence.
Should I see a specialist for diabetic neuropathy?
If your pain isn’t improving after 2-3 months of standard treatment, yes. A neurologist can confirm the diagnosis and rule out other causes. A pain management specialist can offer advanced options like nerve blocks, spinal cord stimulation, or peripheral nerve stimulation. A certified diabetes educator can help you optimize your daily routine. You don’t have to manage this alone.





December 9, 2025 AT 00:01 AM
Look I’ve been diabetic for 18 years and my feet feel like they’re wrapped in barbed wire at night but I’ve been keeping my A1c at 6.8 for two years now and the burning? It’s cut in half. No magic pill just discipline. Stop blaming the meds and start blaming your donuts
December 9, 2025 AT 11:04 AM
THIS. I started walking 20 mins a day and using lidocaine patches before bed 🥹 My toes actually FEEL like they’re there again. I cried last night because I could feel my sock seam. You guys are not alone. 💪🩹
December 11, 2025 AT 05:48 AM
Okay but let’s be real - if you’re still on amitriptyline in 2025 you’re basically living in a 1998 diabetes support group. Duloxetine is the new gold standard. Pregabalin? Sure. But that’s just putting a bandaid on a broken leg. And CBD oil? Please. I’ve seen more snake oil salesmen in my local pharmacy than actual neurologists. If your doctor’s still pushing opioids for neuropathy, fire them. And yes, I’ve read the papers. All of them.
December 12, 2025 AT 15:12 PM
so uhh... you say 'reversal' but then you say 'full reversal is unlikely' so which is it? are we getting a miracle or just a slightly less painful version of hell? also why is everyone acting like TENS units are some kind of divine intervention? I tried one and it felt like my foot was being zapped by a confused bee. also who wrote this? it reads like a pharma brochure with a thesaurus
December 12, 2025 AT 19:46 PM
As someone who has lived with this for over two decades - and who has spoken at three international diabetes conferences - I must emphasize that the most critical factor is not medication, nor even glycemic control alone, but rather the integration of psychoneuroimmunological principles into daily management. The nervous system does not respond to insulin in isolation. It responds to emotional safety, circadian rhythm alignment, and the absence of chronic psychological stress. The fact that this article barely mentions cortisol, or the role of vagal tone, or even the impact of social isolation on pain perception - is, frankly, a disservice to the community. We are not merely biological machines with faulty wiring. We are sentient beings whose pain is amplified by loneliness. And yet, the entire discourse remains fixated on pills and patches. Where is the humanity?
December 13, 2025 AT 17:58 PM
lol at the guy who said 'fire your doctor' - I’ve got a doc who’s been with me since 2012 and he’s the only one who actually listens. also TENS units are kinda magical, ikr? i use mine while watching netflix. no bees. just chill vibes. also walking works. i used to hate it. now i do it with my dog. he’s got neuropathy too. we’re a team 🐶❤️
December 14, 2025 AT 17:38 PM
I just want to say… I’ve been numb for seven years. I lost my big toe last year. I cried in the shower. I didn’t tell anyone. But reading this? I cried again. Not because I’m sad. Because I’m tired. And I’m scared. And I just want someone to tell me it’s okay to not be okay. And that I’m still worthy of healing even if I don’t get it all back.
December 14, 2025 AT 23:08 PM
It is profoundly disappointing that this article, despite its clinical pretensions, fails to cite any primary literature from the last five years. The Diabetes Control and Complications Trial, while seminal, is now over three decades old. One must question the credibility of any medical guidance that relies on outdated evidence - especially when newer studies, such as those published in *Diabetes Care* (2023) on Nav1.7 inhibitors, are entirely omitted. Furthermore, the casual endorsement of TENS units without discussing neural adaptation thresholds or placebo-controlled outcomes borders on medical malpractice. One cannot simply recommend devices without contextualizing their neurophysiological limitations. This is not advice. It is wellness propaganda.
December 16, 2025 AT 14:44 PM
ugh. i read all this. i’m tired. i just want my feet to stop hurting. why does everyone have to be so dramatic about it? i’m on duloxetine. it makes me nauseous. i check my feet. i walk. i hate it. i don’t care about the science. i just want it to stop. why can’t you just say that? why does every post have to be a TED talk?