Most people don’t feel sick when they have metabolic syndrome. No sharp pain. No fever. No cough. Just a slowly growing waistline, a quiet rise in blood pressure, and numbers on a lab report that keep creeping up. By the time symptoms show up - like extreme thirst or blurry vision - the damage is already underway. Metabolic syndrome isn’t one disease. It’s a cluster of three or more warning signs that your body’s metabolism is breaking down. And it’s more common than you think. In Australia, more than 35% of adults have it. In the U.S., it’s nearly one in three. If you’re over 40, overweight, or sedentary, your risk goes up fast.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome is a group of conditions that happen together and raise your risk for heart disease, stroke, and type 2 diabetes. It’s not just about being overweight. It’s about where the fat is stored - and how your body responds to it. The core problem is insulin resistance. That means your muscle, fat, and liver cells stop listening properly to insulin, the hormone that tells your cells to absorb sugar from your blood. So your pancreas pumps out more insulin to compensate. Over time, that leads to high blood sugar, fat buildup, and inflammation.
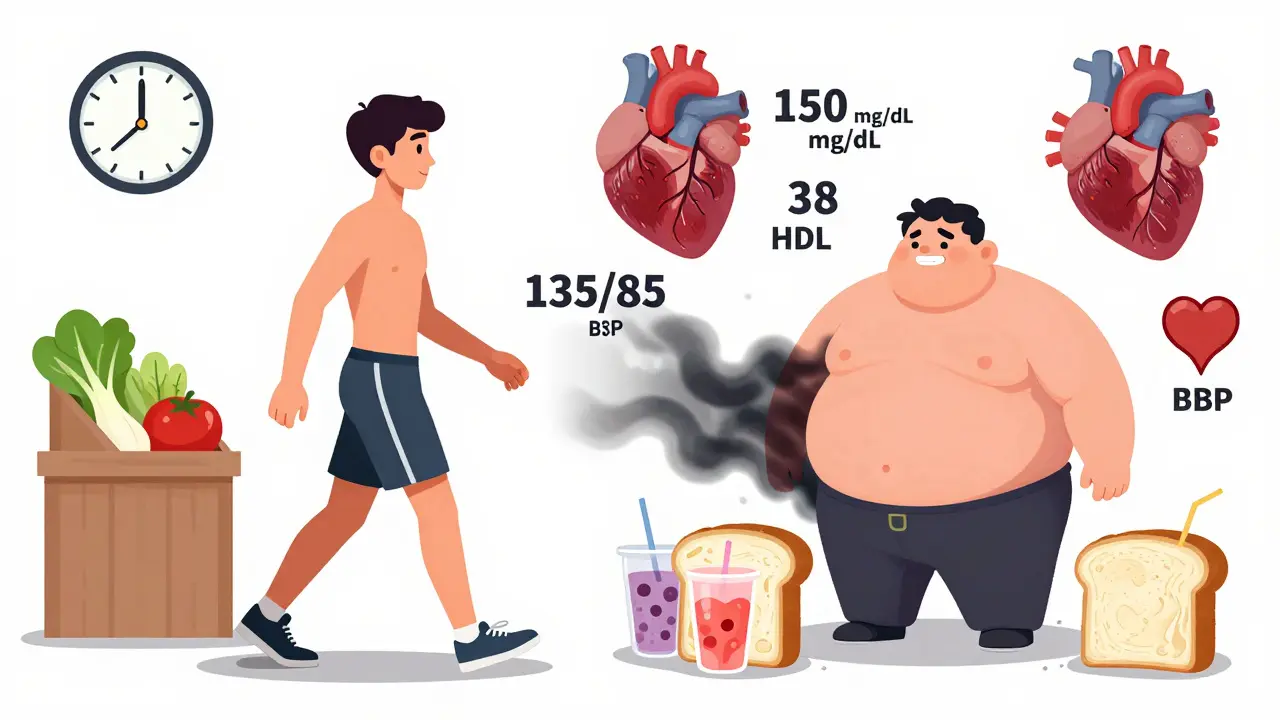
The official diagnosis requires at least three of these five criteria:
- Abdominal obesity: Waist size over 102 cm (40 inches) for men, or 88 cm (35 inches) for women. For people of Asian descent, the thresholds are lower: 90 cm for men, 80 cm for women.
- High triglycerides: 150 mg/dL or higher. This is the fat in your blood that comes from eating too many carbs and sugars.
- Low HDL cholesterol: Below 40 mg/dL for men, below 50 mg/dL for women. HDL is the "good" cholesterol that helps clean out your arteries.
- High blood pressure: 130/85 mmHg or higher, or you’re already on medication for it.
- High fasting blood sugar: 100 mg/dL or higher. This is your blood sugar level after not eating for 8 hours.
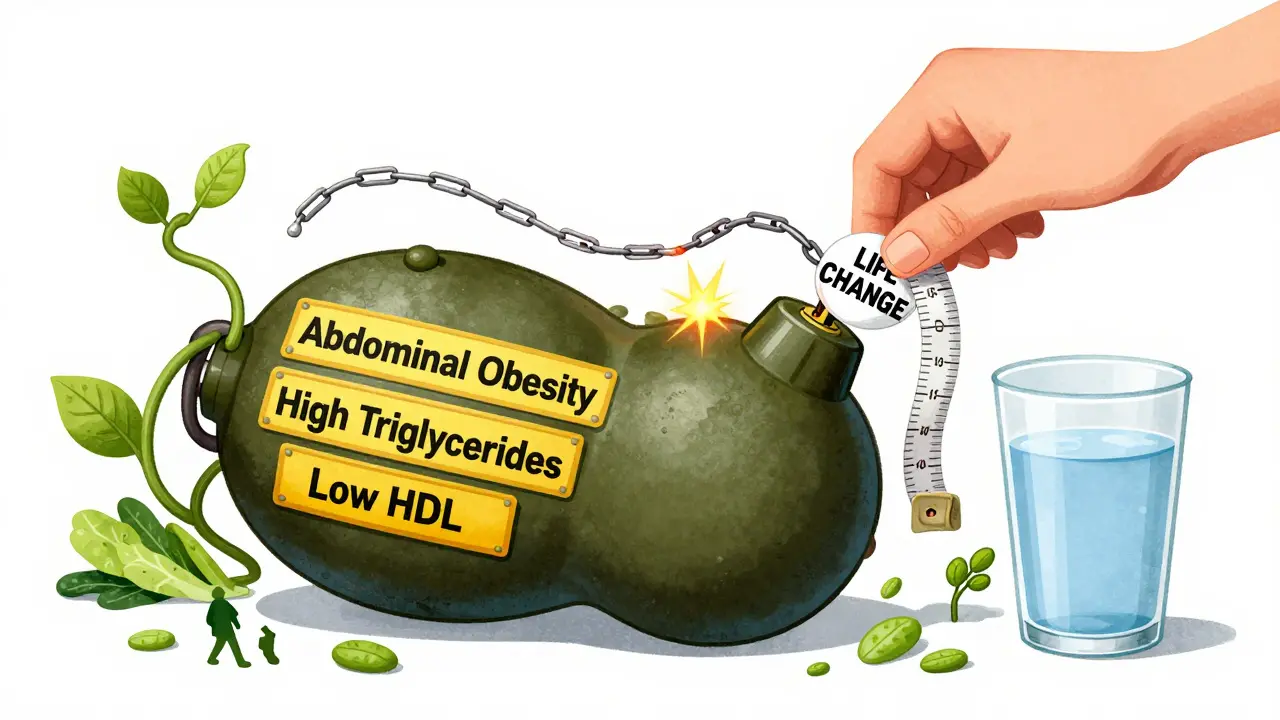
None of these alone is a death sentence. But together? They turn your body into a ticking time bomb. A 2022 study of nearly 3 million people found that metabolic syndrome increases your risk of type 2 diabetes by five times and heart disease by two to three times.
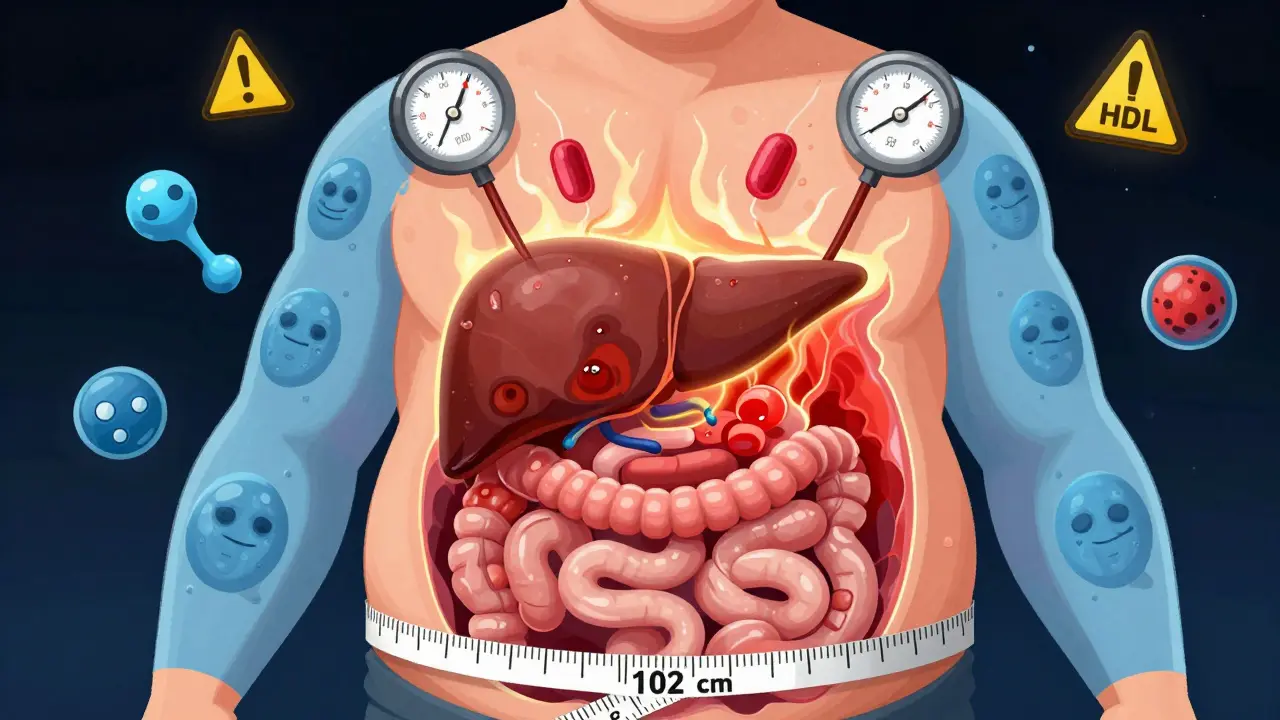
Why Abdominal Fat Is the Real Danger
Not all fat is the same. Fat around your hips and thighs is mostly harmless. But fat inside your belly - the kind that wraps around your liver and intestines - is dangerous. That’s called visceral fat. It’s not just storage. It’s active tissue that releases hormones and inflammatory chemicals directly into your bloodstream.
These chemicals make your cells resistant to insulin. They raise your blood pressure. They make your liver pump out more triglycerides. They lower your HDL. And they don’t just affect your metabolism - they damage your blood vessels over time. That’s why people with a big belly are at higher risk for heart attacks and strokes, even if their overall weight is only slightly above normal.
Doctors measure this with a tape measure, not a scale. A waist size of 94 cm for men or 80 cm for women is already a red flag. By 102 cm or 88 cm, you’re in the metabolic syndrome zone. And it’s not just about looks. It’s about internal damage.
How Blood Pressure and Lipids Connect
High blood pressure and bad lipids don’t happen by accident. They’re both side effects of insulin resistance and inflammation. When your body can’t use insulin properly, your kidneys hold onto more sodium. That increases blood volume and pressure. At the same time, your liver starts making more triglycerides and less HDL. Your blood becomes thicker, stickier, and more prone to clotting.
Triglycerides above 150 mg/dL mean your body is turning excess carbs - especially sugar and refined grains - into fat. That fat doesn’t just sit in your belly. It clogs your arteries. Low HDL is even more telling. It’s like losing your body’s cleaning crew. Without enough HDL, cholesterol builds up in your artery walls. That’s how plaques form. And plaques lead to heart attacks and strokes.
What’s scary is how often these factors go unnoticed. You might have normal blood pressure one year, then 140/90 the next. Your HDL might drop from 55 to 38 without you feeling a thing. That’s why regular check-ups matter. If you’re over 40, or overweight, or have a family history of diabetes, get your waist, blood pressure, and lipid panel checked every year.
Who’s Most at Risk?
Metabolic syndrome doesn’t pick favorites - but it does favor certain groups. The risk jumps with age. Only 20% of people in their 20s have it. By 60, it’s nearly 50%. Women after menopause are especially vulnerable because estrogen drops, and fat shifts from hips to belly.
Ethnicity also plays a role. People of South Asian, Hispanic, African, and Indigenous descent have higher rates, even at lower body weights. That’s why diagnostic thresholds are adjusted for these populations. A waist size of 90 cm might be enough for a South Asian man to qualify, while a Caucasian man needs 102 cm.
Other risk factors? Not moving enough. Eating too many sugary drinks, white bread, and fried foods. Smoking. Sleeping poorly. Having polycystic ovary syndrome (PCOS). And yes - genetics. If your parents had type 2 diabetes or heart disease, your chances go up.
Can It Be Reversed?
Yes. And it doesn’t require drugs - at least not at first. The most powerful treatment is lifestyle change. Not a fad diet. Not a 30-day cleanse. Real, sustainable habits.
Studies show that losing just 5-10% of your body weight can reverse metabolic syndrome in most people. That means if you weigh 90 kg, losing 4.5 to 9 kg makes a huge difference. You don’t need to run marathons. Just 150 minutes of brisk walking per week - that’s 30 minutes, five days a week - cuts your risk significantly.
Food matters more than you think. Cut out sugary drinks. Swap white rice and bread for whole grains. Eat more vegetables, beans, nuts, and fish. Reduce processed snacks. You don’t need to go keto or vegan. Just eat real food. Not packaged food.
One program at Penn Medicine followed 200 people with metabolic syndrome for a year. They got coaching on diet, exercise, and sleep. After 12 months, 65% no longer met the diagnostic criteria. Their blood pressure dropped. Their triglycerides fell. Their HDL rose. Their waistlines shrank. And most didn’t need new medications.
When Medication Becomes Necessary
Lifestyle is the foundation. But sometimes, you need help. If your blood pressure stays high despite diet and exercise, your doctor might prescribe an ACE inhibitor or a calcium channel blocker. If your triglycerides are above 500 mg/dL, they might recommend a statin or fibrates. If your fasting sugar is above 126 mg/dL, metformin might be added to prevent full-blown diabetes.
But here’s the catch: medication treats the numbers, not the cause. If you stop exercising and go back to eating junk, the problems come back. Drugs are a bridge - not a solution. The goal is to get off them by fixing the root problem: insulin resistance.
What Happens If You Ignore It?
Ignoring metabolic syndrome is like ignoring a slow leak in your car’s brake line. Nothing happens right away. Then one day, you hit the pedal - and nothing happens.
Over time, the same processes that cause metabolic syndrome lead to:
- Hardened arteries (atherosclerosis)
- Heart attacks
- Strokes
- Type 2 diabetes
- Non-alcoholic fatty liver disease
- Chronic kidney disease
- Even some forms of cancer
The risk doesn’t just add up - it multiplies. One risk factor? Manageable. Three or more? Your chance of dying from heart disease doubles.
What Should You Do Now?
If you’re reading this, you might be wondering: Do I have it? Here’s what to do next:
- Measure your waist. Stand up. Wrap a tape around your belly, just above your hip bones. If it’s over 94 cm for men or 80 cm for women, pay attention.
- Check your last blood test. Look for triglycerides, HDL, and fasting glucose. If any are out of range, ask your doctor about metabolic syndrome.
- Get your blood pressure checked. Don’t assume it’s fine because you feel okay.
- Start walking 30 minutes a day. Five days a week. No gym needed.
- Replace one sugary drink with water every day. That’s it.
You don’t need to fix everything at once. Just start. Small changes add up. And if you catch it early, you can reverse it. Most people don’t realize how close they are to breaking point - until it’s too late. Don’t wait for symptoms. Check your numbers. Change your habits. Your future self will thank you.


January 12, 2026 AT 01:39 AM
So let me get this straight - we’re telling people to stop eating carbs because some doctor said so? In Nigeria we eat plantain and yam daily and our grandmas live to 90. This is just western fearmongering dressed up as science. You think your 102cm waist is bad? Try walking 10km to market with a bucket on your head. Your insulin resistance is just your body begging for real food not this lab-coat nonsense
January 13, 2026 AT 18:51 PM
Insulin resistance is the core driver but the real issue is chronic hyperinsulinemia from ultra processed foods. The diagnostic criteria are outdated and don't account for ethnic variance in adipose distribution. Also HDL functionality matters more than concentration. Most studies conflate correlation with causation
January 14, 2026 AT 15:53 PM
I see so many people terrified by numbers on a lab report. But here's the truth - you don't need to be perfect. Just move more. Eat one less sugary thing a day. Sleep a little better. Small steps add up. I've seen people reverse this without ever stepping foot in a gym. You're not broken. Your body just needs a little kindness
January 14, 2026 AT 17:32 PM
Yes yes yes. This is the real deal. I was at 110kg and my waist was 108cm. Did 30 min walks every day and swapped soda for water. Lost 12kg in 6 months. My triglycerides dropped from 210 to 98. No meds. Just walking and less junk. You can do this. Start today. Not tomorrow. Today
January 14, 2026 AT 23:37 PM
It's fascinating how visceral fat acts as an endocrine organ - secreting adipokines like leptin and resistin that directly interfere with insulin signaling pathways. The inflammatory cascade initiated by TNF-alpha and IL-6 from abdominal adipose tissue is what drives endothelial dysfunction and subsequent atherosclerosis. This isn't just about appearance - it's systemic metabolic dysregulation
January 16, 2026 AT 19:47 PM
Wait so if I have a 92cm waist but my HDL is 60 and fasting glucose is 85 and BP is 110/70... do I still have metabolic syndrome? Or is it only when you hit three of the five? Asking for a friend who's confused
January 17, 2026 AT 03:40 AM
It is, however, imperative to underscore the fact that the diagnostic criteria for metabolic syndrome, as delineated by the International Diabetes Federation and the National Cholesterol Education Program, are not universally applicable across all ethnic cohorts. The arbitrary thresholds for waist circumference, while statistically significant in majority populations, may not reflect the true pathophysiological thresholds in non-Caucasian individuals. Moreover, the reliance on fasting glucose as a sole indicator of insulin resistance is clinically problematic, given the substantial variability in beta-cell function and hepatic glucose output among individuals.
January 17, 2026 AT 20:17 PM
Look i dont care what your waist size is. I eat rice every day. My uncle had diabetes and he still ate rice. You think this is a western problem? We have real problems here. Corruption. Power outages. No clean water. But you worry about your belly fat? Get real. Your problem is you eat too much kale and think you're better than us
January 18, 2026 AT 04:53 AM
I had metabolic syndrome and I cried for 3 weeks. I looked in the mirror and saw my stomach and I just broke down. My husband left me. My boss said I looked "unprofessional". I went to a nutritionist and she told me to eat more protein. I ate protein. I lost 20kg. But now I'm afraid to eat anything. What if it comes back? What if I'm not enough? I don't know how to live anymore
January 19, 2026 AT 06:47 AM
Metabolic syndrome is just the body screaming for meaning. We've replaced food with consumption. Movement with distraction. Connection with screens. The numbers are just symptoms of a deeper spiritual decay. You can't fix insulin resistance with kale. You fix it with presence. With stillness. With remembering you're not a machine to be optimized
January 19, 2026 AT 11:13 AM
There's a quiet dignity in the way our bodies signal distress before they break. No alarm bells. No dramatic collapse. Just a slow unraveling. We've built a world that rewards busyness over being. Efficiency over presence. And our biology pays the price in silent, invisible ways. Perhaps the real revolution isn't in the gym or the kitchen - but in learning to listen again
January 20, 2026 AT 23:11 PM
So you think walking 30 minutes fixes everything? My cousin walked 5km to work every day and still got diabetes. You think it's about movement? It's about food. Real food. Not this western processed crap. We don't need your advice. We need your respect
January 22, 2026 AT 15:24 PM
Just lost 15kg in 4 months. No diet. Just stopped eating after 7pm. My waist went from 106 to 89. My BP is normal now. I didn't even know I had this. Just started walking to the store instead of driving. You don't need a plan. Just start