Beta-Blocker Hypoglycemia Risk Comparison
Hypoglycemia Risk Comparison
When using insulin therapy, different beta-blockers affect hypoglycemia awareness differently. This tool compares the risk profiles of common beta-blockers based on research findings.
| Beta-Blocker Type | Typical Agents | Hypoglycemia Risk | Symptom Masking | Recommendation |
|---|---|---|---|---|
| Non-selective | Propranolol, Nadolol |
High Risk (OR 2.3) |
Mask most adrenergic signs (tachycardia, tremor) | Use only if absolutely necessary; avoid in patients with hypoglycemia unawareness |
| Cardioselective | Metoprolol, Atenolol |
Moderate Risk (OR 1.87) |
Mask many signs, some sweating remains | Prefer at low doses; monitor closely |
| Mixed (Carvedilol) | Carvedilol |
Lowest Risk (OR 1.21) |
Partial masking, better glucose recovery | Preferred choice when beta-blockers are needed |
Understanding the Risk Profiles
Odds ratios (OR) indicate the relative risk of hypoglycemia compared to no beta-blocker use. An OR of 1.0 means no increased risk. Higher numbers mean greater risk.
Even with beta-blockers, sweating usually remains intact because it's driven by acetylcholine rather than the beta-adrenergic pathway. This makes unexpected sweating a critical warning sign to monitor for.
When choosing a beta-blocker for patients on insulin, carvedilol is the preferred option due to its lower risk profile and potential benefits for glucose recovery. Avoid non-selective agents when possible.
Key Clinical Recommendations
When starting a beta-blocker: Lower basal insulin by 10-20% and increase glucose monitoring frequency (every 2-4 hours initially).
For patients already on beta-blockers: Educate about sweating as the primary remaining warning sign of hypoglycemia.
Consider continuous glucose monitoring (CGM): Usage has risen 300% since 2018 and has reduced severe episodes by 42% in patients on beta-blockers.
When a person with diabetes takes insulin while also needing a beta‑blocker for heart or blood‑pressure reasons, the mix can turn a routine day into a dangerous one. The main problem? hypoglycemia unawareness-the loss of the usual warning signs that blood sugar is dropping too low.
What is hypoglycemia unawareness?
Hypoglycemia unawareness is a condition where the brain’s alarm system stops shouting when glucose falls below the safe level. Instead of feeling shaky, sweaty, or having a racing heart, the person may only notice confusion or loss of consciousness. Studies show about 40% of people with type 1 diabetes develop this, while it’s less common in type 2 diabetes.
Why beta‑blockers matter
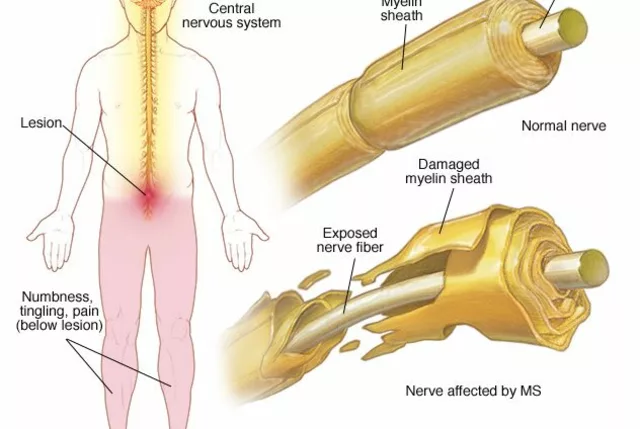
Beta‑blockers are medicines that slow the heart and lower blood pressure by blocking adrenaline receptors. They are a go‑to for patients who have had a heart attack, need blood‑pressure control, or suffer from certain rhythm problems. The catch is that adrenaline (especially the beta‑1 and beta‑2 signals) creates many of the classic hypoglycemia symptoms-fast heartbeat, tremor, anxiety. When a beta‑blocker dampens those signals, the early alerts disappear.
How insulin and beta‑blockers interact
Insulin is the hormone that pulls glucose into cells, lowering blood sugar. In people who inject insulin, a mis‑dose or a missed meal can quickly push glucose into the danger zone. Add a beta‑blocker, and the body’s natural “call‑to‑action” (release of glucose from the liver and muscles) is also blunted. Research by Carnovale (2021) showed that beta‑2 blockade reduces glycogenolysis, meaning the liver can’t crank out sugar fast enough to recover.
Which beta‑blockers are riskier?
Not all beta‑blockers behave the same. Two broad groups dominate:
- Cardioselective beta‑blockers (also called selective beta‑blockers) mainly block the beta‑1 receptor found in the heart. Examples include metoprolol and atenolol.
- Non‑selective beta‑blockers block both beta‑1 and beta‑2 receptors. Propranolol is the classic example.
Data from Dungan (2019) indicated that non‑selective agents raise the odds of hypoglycemia about 2.3‑fold compared with no beta‑blocker, while selective agents still increase risk but less dramatically. Carvedilol, a mixed‑alpha/beta blocker, seems to sit in the middle-its alpha‑blocking action causes vasodilation, which may improve glucose delivery and lower the hypoglycemia odds (OR 1.21 vs. 1.87 for selective agents).
| Beta‑blocker type | Typical agents | Effect on hypoglycemia symptoms | Hospital‑study odds ratio* |
|---|---|---|---|
| Non‑selective | Propranolol, nadolol | Mask most adrenergic signs (tachycardia, tremor) | 2.3 |
| Selective (beta‑1) | Metoprolol, atenolol | Mask many signs, some sweating remains | 1.87 |
| Mixed (carvedilol) | Carvedilol | Partial masking, better glucose recovery | 1.21 |
*Odds ratios from Dungan 2019, hospitalized diabetic patients not on basal insulin.

What still works as a warning sign?
Even if beta‑blockers hide the classic adrenaline‑driven clues, sweating usually stays intact because it’s driven by acetylcholine, not norepinephrine. That means a cold‑clammy skin patch can still be the only clue. Teaching patients to check for unexpected sweat, especially on the palms or forehead, is a lifesaver.
Guidelines that shape practice
Both the American Diabetes Association (2023) and the American Heart Association (2022) acknowledge the double‑edge sword:
- Continue cardioselective beta‑blockers when the heart‑protective benefit outweighs risk.
- Intensify glucose monitoring-check blood sugar every 2‑4 hours in the hospital, and consider continuous glucose monitoring (CGM) for out‑patients.
- Avoid non‑selective agents in patients who already have hypoglycemia unawareness.
In the outpatient world, CGM has exploded-usage rose 300 % since 2018 among diabetics on beta‑blockers, slashing severe episodes by roughly 42 % (T1D Exchange Registry).
Practical steps for clinicians
- Identify risk early. Review the medication list at every visit. Flag anyone on insulin plus a beta‑blocker.
- Choose the safest beta‑blocker. If a beta‑blocker is essential, prefer carvedilol or a low‑dose cardioselective agent.
- Adjust insulin doses. When starting a beta‑blocker, lower basal insulin by 10‑20 % and monitor response.
- Educate about sweating. Show patients how to feel for unexpected dampness on the neck or upper back.
- Implement frequent monitoring. For in‑patients, order point‑of‑care glucose checks every 3 hours. For out‑patients, prescribe a CGM or at least 7‑point finger‑stick profiles.
- Document hypoglycemia episodes. Use the hospital’s safety reporting system; trends help tweak therapy.
- Re‑evaluate continuously. If a patient develops hypoglycemia unawareness, consider switching to an alternate antihypertensive class (e.g., ACE inhibitor) if feasible.

Patient‑focused education checklist
- Explain that beta‑blockers can hide warning signs.
- Teach the “sweat‑first” rule: any sudden cold sweat = check glucose.
- Provide a written log sheet for glucose readings and any symptoms.
- Show how to use a CGM receiver or smartphone app.
- Stress the importance of eating regular meals and carrying fast‑acting carbs.
- Encourage a partner or family member to be aware of the risk.
Emerging research and future directions
Scientists are hunting ways to restore hypoglycemia awareness. Small studies suggest that β‑adrenergic agonists, methylxanthines (like caffeine), and even low‑dose opiate antagonists can “wake up” the brain’s alarm system. The DIAMOND trial (2023) is testing genetic markers that predict who will develop beta‑blocker‑related hypoglycemia, aiming for precision prescribing.
Until those tools are ready, the best defense remains vigilant monitoring and smart drug selection.
Bottom line for safe insulin‑beta‑blocker therapy
Combining insulin with any beta‑blocker raises the stakes for hidden hypoglycemia. The safest approach is:
- Prefer cardioselective or mixed agents like carvedilol over non‑selective drugs.
- Increase glucose‑checking frequency, especially during the first 24 hours after a new prescription.
- Educate patients that sweating may be the only leftover signal.
- Use CGM wherever possible to catch drops before they become severe.
- Re‑assess the need for a beta‑blocker if hypoglycemia unawareness persists.
Follow these steps, and you can keep the heart‑protective benefits of beta‑blockers without letting silent hypoglycemia take you by surprise.
Can non‑selective beta‑blockers cause low blood sugar by themselves?
They don’t lower glucose directly, but they block the adrenaline signals that normally raise blood sugar during a hypoglycemic episode. That masking effect can let a drop go unnoticed and become more severe.
Is sweating still a reliable sign when I’m on a beta‑blocker?
Yes. Sweating is driven by acetylcholine, not the beta‑adrenergic pathway, so it usually remains intact. Teach patients to treat unexpected sweat as a cue to check glucose.
Should I switch from metoprolol to carvedilol if I have type 1 diabetes?
If you need a beta‑blocker for heart protection, carvedilol often carries a lower hypoglycemia risk. Discuss the switch with your cardiologist and endocrinologist together.
How often should I check my blood sugar after starting a beta‑blocker?
During the first 24‑48 hours, aim for a check every 2‑3 hours (or use a CGM). After you’ve settled into a stable pattern, every 4‑6 hours is usually enough, but always follow your doctor’s plan.
Are there any alternatives to beta‑blockers for blood‑pressure control in diabetics?
ACE inhibitors, ARBs, and certain calcium‑channel blockers are effective and don’t interfere with hypoglycemia awareness. The choice depends on your heart‑health profile.



October 25, 2025 AT 12:57 PM
They hide the sugar drop on purpose, a pharma scam!
October 26, 2025 AT 15:44 PM
Imagine a world where medicine protects the heart but blinds the mind to the danger we rely on intuition it forces us to rethink trust in prescriptions
October 27, 2025 AT 19:30 PM
In clinical practice the selection of a beta‑blocker must be guided by a comprehensive risk‑benefit assessment particularly in insulin‑treated patients
October 28, 2025 AT 23:17 PM
i cant believe docs still prescribe non‑selective betas to type 1 peeps it's like they forgot about hypoglycemia unawareness lol the sweat clue is the only thing left
October 30, 2025 AT 03:04 AM
Such reckless prescribing betrays the sanctity of patient safety, a tragedy befitting a melodrama of modern medicine. The veil of beta‑blockade drapes over the fragile equilibrium of glucose homeostasis.
October 31, 2025 AT 06:50 AM
🌟 Remember, a cold sweat can mean you’re dropping low – check your glucose right away! 📲 Stay safe and share this tip with anyone on insulin + beta‑blockers 😊
November 1, 2025 AT 10:37 AM
You’re absolutely right that the combination of insulin and beta‑blockers turns monitoring into a high‑stakes game. When the adrenaline alarm is muted, patients can slip into severe hypoglycemia without the usual shaky warning. Sweating remains a reliable sign because it is mediated by acetylcholine, and teaching patients to notice unexpected clammy skin is essential. Frequent glucose checks, especially every two to three hours during the first day of a new beta‑blocker, can catch drops early. Continuous glucose monitors have truly changed the landscape, offering real‑time alerts that bypass the hidden symptoms. Studies showing a 42 % reduction in severe episodes with CGM underscore how technology can compensate for physiological blind spots. Adjusting basal insulin by 10‑20 % when starting a beta‑blocker is a sensible precaution that many clinicians overlook. Collaborating with cardiologists to choose a cardio‑selective or mixed agent like carvedilol can preserve heart benefits while lowering hypoglycemia risk. Educating family members to recognize the sweat‑first rule adds an extra layer of safety, especially for those living alone. Documenting every hypoglycemic event in the medical record helps identify patterns and guide future medication tweaks. If unawareness persists despite these measures, it may be time to explore alternative antihypertensives such as ACE inhibitors. The emerging research on β‑adrenergic agonists and caffeine as awareness‑restoring agents is intriguing, though still early. Precision prescribing based on genetic markers, as the DIAMOND trial is pursuing, could eventually personalize therapy. Until those tools are widely available, vigilance remains our best defense. Keep the conversation going with your care team, and never hesitate to ask for a CGM trial if you feel at risk.
November 2, 2025 AT 14:24 PM
They don’t want you to know that big pharma hides the truth about beta‑blockers and sugar drops the elite decide who gets safe meds
November 3, 2025 AT 18:10 PM
Even with that hidden risk there’s hope – new tech and studys are making it easier to spot low sugar before it becomes danger :)
November 4, 2025 AT 21:57 PM
From a broader perspective, integrating cardiovascular care with diabetes management reflects a holistic approach that respects both heart health and glucose stability.
November 6, 2025 AT 01:44 AM
Let’s push for stricter guidelines now – patients deserve clear protocols that prevent silent hypoglycemia while preserving heart protection.
November 7, 2025 AT 05:30 AM
Practical tip: set your CGM alerts at 80 mg/dL and review trends daily to stay ahead of any hidden drops
November 8, 2025 AT 09:17 AM
Stop ignoring the danger!
November 9, 2025 AT 13:04 PM
The article repeats old data without offering new solutions.