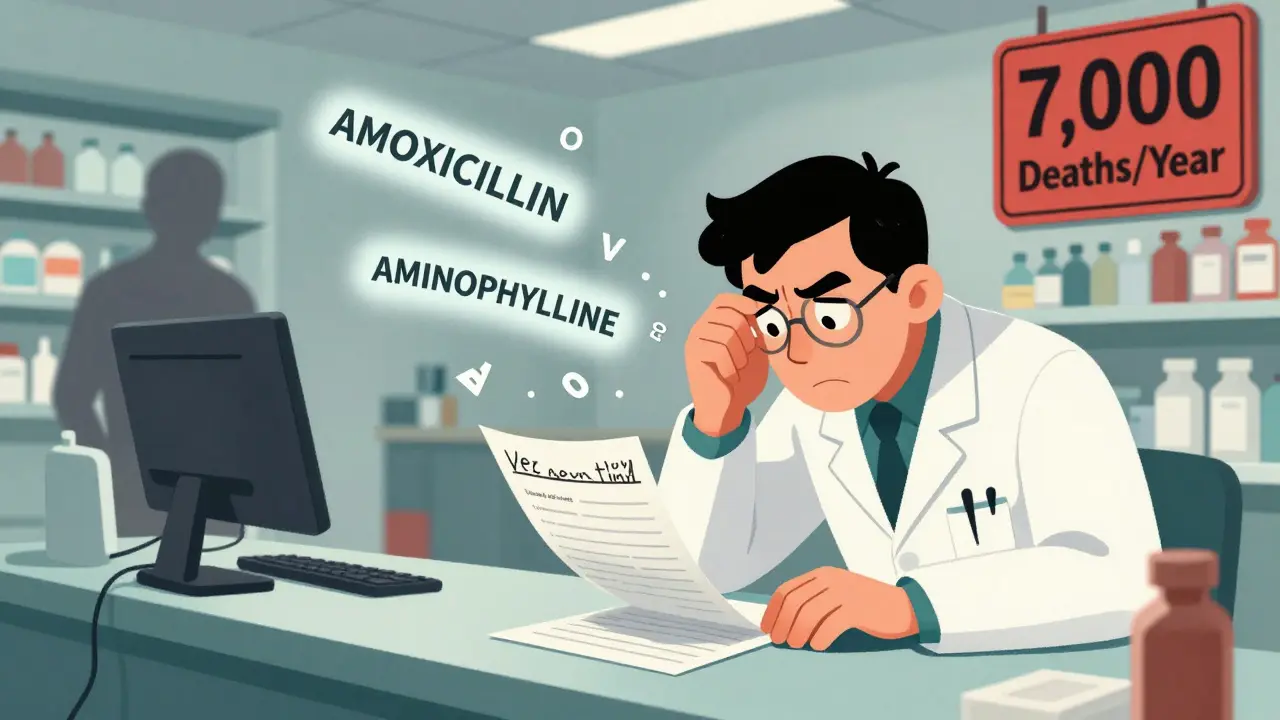
Imagine this: a pharmacist stares at a scribbled prescription, squinting at a barely legible scrawl that might say amoxicillin-or maybe aminophylline. One letter wrong. One dose misunderstood. And suddenly, a patient is in the ER because of a mistake that never should’ve happened. This isn’t fiction. It’s real. Every day, thousands of prescriptions around the world are misread because of poor handwriting. And the consequences? They can be deadly.
Why Illegible Handwriting Is a Silent Killer
In the U.S. alone, an estimated 7,000 people die each year because of prescription errors caused by handwriting that’s too hard to read. That’s not a typo. That’s 7,000 lives lost to something that’s been fixable for over two decades. The Institute of Medicine first flagged this in the early 2000s, calling handwritten prescriptions a "dinosaur long overdue for extinction." Back then, many doctors still wrote prescriptions by hand, often under time pressure, juggling multiple patients, charting notes, and answering pages-all while trying to write fast enough to keep up. The problem isn’t just messy penmanship. It’s the missing pieces: no prescriber initials, wrong dosage units (like writing "10 mg" instead of "10 mL"), ambiguous abbreviations like "QD" (which some read as daily, others as every other day), or unclear routes of administration. A 2005 study in a British hospital found that only 24% of handwritten operative notes were rated as "excellent" or "good" by nurses and medical staff. Nearly 40% were labeled "poor." That’s not a glitch. That’s a system failure. Pharmacists are on the front lines. In the U.S., they make about 150 million phone calls every year just to clarify prescriptions. Each call delays treatment. Each delay increases risk. Nurses, too, spend an average of 12.7 minutes per illegible prescription tracking down the right info. That’s over 12 minutes of time that could’ve gone to patient care-time lost to a pen stroke. And it’s not just busy professionals. A 2022 study found that 92% of medical students and doctors had made at least one prescription error due to handwriting. Shockingly, 22% of them admitted they’d sometimes just guess what was written-and move on. That’s not negligence. It’s survival. When you’re overwhelmed, you do what you have to do. But when you guess wrong, someone could die.How E-Prescribing Fixed the Problem
The solution wasn’t more training. It wasn’t better pens. It was technology. Electronic prescribing, or e-prescribing, began rolling out in the early 2000s. By 2019, 80% of office-based providers in the U.S. had switched over. And the results? Dramatic. A 2025 study in JMIR found that e-prescriptions had an 80.8% accuracy rate in meeting safety standards. Handwritten ones? Just 8.5%. That’s a 9.5x improvement. Even manually typed e-prescriptions-without templates or auto-fill-still hit a 56% accuracy rate. That’s still better than handwriting by a landslide. E-prescribing eliminates the guesswork. No more confusing "U" for units (which looks like a zero). No more "cc" instead of "mL." No more ambiguous "q.i.d." or "b.i.d." The system forces you to pick from standardized options: drug name, dose, frequency, route, duration. It flags potential allergies, drug interactions, and duplicate therapies before the prescription even leaves the screen. Veradigm reports e-prescribing reduces errors from illegibility by 97%. That’s not marketing speak. That’s data. One doctor in Sydney told me his pharmacy used to call him five times a day. After switching to e-prescribing, it dropped to once a month. And not because he got better at writing. Because he stopped writing at all.The Hidden Costs of Going Digital
But e-prescribing isn’t magic. It’s not perfect. And it didn’t come without trade-offs. First, the cost. Setting up a full system can run $15,000 to $25,000 per provider. Training staff takes 8 to 12 hours per clinician. Integrating with existing electronic health records? That’s a project in itself. Smaller clinics, especially in rural or low-resource areas, still struggle with this. Then there’s alert fatigue. E-prescribing systems bombard doctors with warnings: "This drug interacts with your patient’s blood pressure med." "This dose exceeds the maximum daily limit." "This patient is allergic to this class." Sounds good-until you get 15 alerts per prescription, and 14 of them are irrelevant. Clinicians start ignoring them. And that’s when the danger returns. A 2025 study warned that if alerts aren’t smart, they become noise. The system has to learn. It has to prioritize. It can’t scream about every tiny risk. It has to focus on the ones that actually matter. And then there’s the human factor. Some doctors still feel like e-prescribing slows them down. They miss the speed of scribbling a note. But the truth? The time saved by avoiding phone calls, correcting errors, and redoing prescriptions adds up. One study found that after switching, doctors actually spent less time overall on prescribing tasks.
What If You Can’t Go Digital?
Not every clinic can afford e-prescribing. Not every country has the infrastructure. So what do you do if you’re still writing by hand? There are still ways to reduce risk.- Print, don’t write in cursive. Block letters are easier to read. No loops. No flourishes.
- Avoid dangerous abbreviations. Never use "U" for units. Never use "QD," "QOD," or "cc." Use "daily," "every other day," and "mL." The Joint Commission has a full "Do Not Use" list. Use it.
- Write everything. Patient name. Drug name. Exact dose. Frequency. Route. Duration. Prescriber name and contact info. No shortcuts.
- Use printed templates. Some clinics use pre-printed prescription pads with boxes to fill in. It forces structure.
- Self-check with a checklist. A 2019 study showed that doctors who used a 15-item checklist before signing prescriptions reduced errors by 40%.
The Future Is Already Here
By 2030, handwritten prescriptions will be rare in developed countries. The U.S., Australia, Canada, and the U.K. are already there. Regulatory pressure is pushing it further. The Medicare Improvements for Patients and Providers Act of 2008 gave financial incentives. The 21st Century Cures Act of 2016 demanded interoperability. Now, Medicare and Medicaid won’t reimburse for handwritten scripts in most cases. Emerging tech is helping too. AI-powered handwriting recognition tools can now interpret 85-92% of common medication names from scanned paper scripts. That’s not a replacement for e-prescribing-but it’s a bridge. For clinics still using paper, it can cut down on misreads and reduce calls to doctors. But the real win isn’t the tech. It’s the culture shift. Doctors, pharmacists, and nurses are no longer accepting sloppy handwriting as "just part of the job." It’s seen for what it is: a preventable cause of harm. Dr. Cheryl Reifsnyder from Veradigm put it simply: "E-prescribing has absolutely lived up to expectations in improving patient safety." And she’s right. We didn’t need to train doctors to write better. We needed to stop asking them to write at all.
What You Can Do
If you’re a patient: Ask your doctor if they use e-prescribing. If they don’t, ask why. If they still write prescriptions, make sure you can read every part of it. If you can’t, say so. Don’t assume the pharmacist will figure it out. If you’re a clinician: If you haven’t switched to e-prescribing yet, consider the cost of staying with paper-not just in dollars, but in lives. The time you save on clarifying errors adds up. The mistakes you avoid? They’re priceless. If you’re a policymaker or administrator: Invest in digital infrastructure. Don’t wait for a tragedy to force your hand. The data is clear. The solution exists. The only question is: are you ready to act?Final Thought
Illegible handwriting on prescriptions isn’t a minor inconvenience. It’s a systemic flaw that cost thousands of lives. And we fixed it-not with better pens, not with stricter rules, but by removing the pen entirely. That’s not just innovation. That’s responsibility.How many deaths are caused by illegible handwriting on prescriptions?
An estimated 7,000 preventable deaths occur each year in the United States due to prescription errors caused by illegible handwriting, according to data from the Institute of Medicine and Veradigm. These errors include misread dosages, wrong drug names, and incorrect administration instructions.
What is e-prescribing and how does it improve safety?
E-prescribing is the electronic transmission of prescriptions from a clinician to a pharmacy using a digital system. It improves safety by eliminating handwriting errors, auto-filling correct dosages, flagging drug interactions, preventing dangerous abbreviations, and ensuring all required information is included. Studies show e-prescriptions have an 80.8% safety compliance rate, compared to just 8.5% for handwritten ones.
Are handwritten prescriptions still allowed?
Yes, but they’re increasingly rare in developed countries. In the U.S., Medicare and Medicaid now require e-prescribing for most prescriptions to qualify for reimbursement. Some rural or low-resource clinics still use paper, but regulatory trends and patient safety standards are pushing toward full digital adoption by 2030.
What are the most dangerous abbreviations in handwritten prescriptions?
Dangerous abbreviations include: "U" for units (can be mistaken for "0" or "4"), "QD" for daily (can be read as "QID" for four times daily), "QOD" for every other day (can be misread as daily), "cc" for cubic centimeters (should be mL), and "MS" for morphine sulfate (can be mistaken for magnesium sulfate). The Joint Commission’s "Do Not Use" list bans these and others.
How much time do nurses spend clarifying illegible prescriptions?
Nurses spend an average of 12.7 minutes per illegible prescription tracking down correct information. In busy hospitals, that adds up to hours of lost time each day-time that could be spent directly caring for patients.
Can AI help read handwritten prescriptions?
Yes. Early AI tools for handwriting recognition can interpret 85-92% of common medication names from scanned paper prescriptions. While not a full replacement for e-prescribing, these tools help reduce errors in settings where digital systems aren’t yet available.
What’s the biggest challenge with e-prescribing systems?
The biggest challenge is alert fatigue-when clinicians are overwhelmed by too many safety warnings, many of which aren’t critical. This leads to important alerts being ignored. Smart systems now use machine learning to prioritize only the most dangerous interactions, reducing noise while keeping safety high.
How much does it cost to switch to e-prescribing?
The average cost for a full e-prescribing system is $15,000 to $25,000 per provider, including software, training, and integration with electronic health records. Staff training typically takes 8-12 hours per clinician. While expensive upfront, the long-term savings from reduced errors and fewer phone calls often pay for the system within a year.



January 22, 2026 AT 11:36 AM
I never realized how much time nurses waste just trying to read prescriptions. I had my grandma on antibiotics last year, and the pharmacist called three times just to confirm the dose. It’s insane that we’re still relying on handwriting in 2025. I’m glad e-prescribing is catching on, but why does it take a tragedy to change something so basic?
January 24, 2026 AT 02:22 AM
7000 deaths a year from bad handwriting? Bro. We’re not in the 1800s. This is just lazy medicine. Doctors need to get with the program or get out. No more excuses. Stop writing. Start typing. Done.
January 25, 2026 AT 13:57 PM
Let’s be real - this isn’t about handwriting. It’s about doctors being overworked and underpaid. They’re scribbling because they’re running on fumes. Fix the system, not the pen. E-prescribing helps, but if you’re still making 30 patients a day with no support staff, you’re gonna write messy. Blame the grind, not the pen.
January 26, 2026 AT 22:35 PM
Alert fatigue?? That’s the real problem!! E-prescribing systems are designed by people who’ve never seen a 3 a.m. ER shift. They throw 20 alerts at you for every script - half of them are ‘this drug might interact with something your patient took in 2018.’ It’s not safety - it’s noise pollution. And now we ignore the real ones. That’s worse than bad handwriting.
January 28, 2026 AT 00:30 AM
The 80.8% safety compliance rate for e-prescriptions versus 8.5% for handwritten is statistically overwhelming. The delta is not merely significant - it is clinically transformative. The reduction in medication error incidence correlates directly with system adoption, per JMIR’s 2025 cohort analysis. Structural interventions outperform behavioral ones in high-stakes environments. Ergo, the pen is obsolete.
January 28, 2026 AT 07:37 AM
They say e-prescribing saves lives... but what if it’s just Big Pharma’s way of controlling your meds? 🤔 You ever wonder who owns the algorithm that decides what drugs get flagged? What if they’re hiding side effects? And why do all the alerts disappear when you’re on Medicare? 👀 #BigMedicineIsWatching
January 29, 2026 AT 16:10 PM
USA is the only country that’s still debating this. Canada switched in 2010. UK in 2015. Australia? Done. We’re still acting like we’re in the Stone Age because some old doc says he ‘misses writing.’ Get over it. Your ego isn’t worth someone’s life. And if your clinic can’t afford it? That’s your problem - not the patient’s.
January 31, 2026 AT 09:43 AM
It’s not just about safety - it’s about dignity. When you handwrite a script, you’re treating your patient like an afterthought. You’re saying, ‘I’m too tired to be clear.’ E-prescribing isn’t tech - it’s ethics. It’s saying, ‘Your life matters enough for me to type this properly.’ And if you’re still scribbling? You’re not a doctor. You’re a relic.
February 2, 2026 AT 08:23 AM
My aunt died because of a misread script. Never again.
February 3, 2026 AT 06:35 AM
It is imperative that all healthcare providers transition to electronic prescribing systems without further delay. The empirical evidence is unequivocal. Continued reliance upon handwritten prescriptions constitutes a breach of the standard of care. I urge regulatory bodies to enforce compliance with immediate effect.
February 4, 2026 AT 04:46 AM
One cannot help but observe that the cultural inertia surrounding the persistence of handwritten prescriptions reflects a broader societal failure to prioritize precision in medical practice. The aesthetic of the handwritten note - romanticized as ‘personal’ - is, in fact, a dangerous anachronism. The clinical environment demands rigor, not nostalgia.
February 5, 2026 AT 06:29 AM
Oh wow, 7000 deaths? Guess that’s why they call it ‘the American healthcare system.’ We fix the symptom, not the disease. Meanwhile, insurance companies charge $800 for a Band-Aid. But hey, at least your prescription won’t be smudged. 🙃
February 6, 2026 AT 05:28 AM
Here in India, we still use paper scripts - but we’ve got a trick: we write the drug name in capital letters, and the dose in numbers. No abbreviations. And we always write our phone number. It’s not fancy, but it works. And yeah, we still get calls from pharmacies… but fewer than before. 🙏