It’s 2025, and nearly 90% of all prescriptions filled in the U.S. are for generic drugs. That’s not just a cost-saving trend-it’s the new standard. But if you’ve ever switched from a brand-name pill to a generic and suddenly felt off, you’re not alone. Many people swear their generic version doesn’t work the same, causes more side effects, or even triggers unexpected interactions. The truth? Most of the time, it’s not the drug itself. It’s what’s hiding in the pill.
Why Do People Think Generics Interact Differently?
The idea that generics behave differently from brand-name drugs is widespread. On Reddit, pharmacy forums, and even in doctor’s offices, patients say things like: “My old brand kept my INR steady, but this new generic made me dizzy.” Or: “I’ve never had stomach issues with my levothyroxine until I switched.” Here’s the reality: the active ingredient in a generic drug must be identical to the brand-name version. The FDA requires it. That means if you’re taking a generic version of simvastatin, it’s the exact same molecule as the brand-name Zocor. It works the same way in your body. It’s metabolized the same. It interacts with other drugs the same. So why do people report differences? Three main reasons:- Inactive ingredients-the fillers, dyes, and binders-are different. A generic levothyroxine might use lactose, while the brand uses corn starch. If you’re lactose intolerant, that’s not a drug interaction-it’s a food sensitivity triggering nausea or bloating.
- Nocebo effect-if you believe generics are inferior, your brain can convince your body you’re feeling worse. Studies show patients report more side effects when they know they’re taking a generic, even when the pill is identical to the brand.
- Switching manufacturers-if your pharmacy switches from one generic maker to another, the inactive ingredients change again. One batch might have a different coating, another a different lubricant. Your body notices the difference, even if the active drug doesn’t.
What Actually Causes Real Drug Interactions?
Drug interactions aren’t about whether a pill is generic or brand-name. They’re about the chemistry of the active ingredient and how it behaves in your body. There are three types of real, documented interactions:- Drug-drug: Fluconazole (an antifungal) can spike simvastatin levels by 300-400%, raising the risk of muscle damage. This happens whether the simvastatin is generic or brand.
- Drug-food: Grapefruit juice blocks an enzyme called CYP3A4. That means it can make blood pressure meds like amlodipine or cholesterol drugs like atorvastatin build up to dangerous levels. Again, this affects all versions of the drug equally.
- Drug-condition: Diphenhydramine (Benadryl) can raise eye pressure in people with glaucoma. It doesn’t matter if it’s the generic or the name brand-it’s the same compound.
The Real Culprit: Inactive Ingredients
Here’s where things get tricky. While the active ingredient is locked in, the inactive ones? Not so much. Generic manufacturers can-and often do-change excipients between batches. That’s legal. It’s also cost-effective. But for some people, it matters. Take sertraline, a common antidepressant. The brand-name Zoloft uses hydrochloride as a salt form. Some generics use sodium benzoate instead. In rare cases, sodium benzoate can interact with acidic foods or other medications in sensitive individuals, causing mild nausea or headaches. It’s not the antidepressant working differently-it’s the additive. Another example: levothyroxine. In 2021, a patient in a Journal of the American Pharmacists Association case report had severe GI upset after switching to a generic version. The brand used no lactose. The generic did. Once switched back, symptoms vanished. These aren’t drug interactions in the traditional sense. They’re allergic or intolerance reactions to fillers. But they feel just as real to the patient.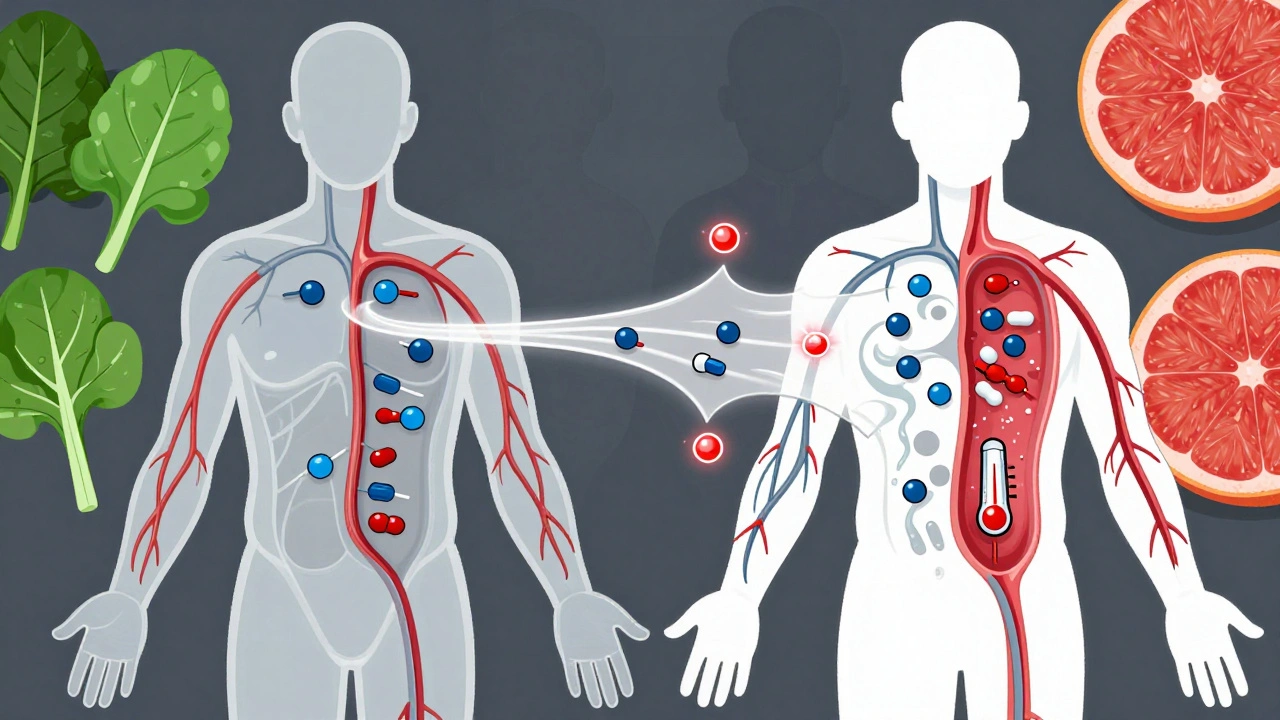
Narrow Therapeutic Index Drugs: When Even Small Changes Matter
Some drugs have a razor-thin margin between “effective” and “toxic.” These are called narrow therapeutic index (NTI) drugs. For these, even tiny differences in how the body absorbs the drug can be dangerous. Examples include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin (seizure medication)
- Digoxin (heart medication)
What Should You Do?
If you’ve noticed a change after switching to a generic, don’t panic. But don’t ignore it either. Here’s what to do:- Check the label. Look at the “inactive ingredients” section. If you’re allergic to lactose, gluten, or certain dyes, compare the generic and brand names. The list should be on the packaging or available from your pharmacist.
- Don’t switch manufacturers randomly. If you’re on warfarin or levothyroxine, ask your pharmacist to stick with the same generic brand. Consistency matters more than cost here.
- Track your symptoms. Keep a simple log: date, medication, dose, symptoms. Did the issue start right after the switch? Did it stop when you went back? That’s valuable data for your doctor.
- Ask your pharmacist. They know which generics come from which manufacturers. They can tell you if your current pill has a different filler than your last one.
- Don’t assume it’s “all in your head”. If you feel different, it’s real-even if the cause isn’t the active drug. Your body is responding to something.

The Bigger Picture: Perception vs. Reality
A 2022 Kaiser Family Foundation survey found 47% of patients believe generics work differently than brand-name drugs. But when researchers checked actual medical records, only 3.7% of those reports had any physiological basis. The rest? Misunderstandings. Nocebo effects. Switching between different generics. Dietary changes. Stress. Sleep loss. All things that affect how you feel-but aren’t caused by the drug itself. Meanwhile, the FDA’s post-marketing data shows only 0.03% of adverse event reports for generics cite unexpected interactions. That’s less than 1 in 3,000. For brand-name drugs? The rate is nearly identical. The real problem isn’t the science. It’s the myth.What’s Changing in 2025?
The FDA launched a pilot AI program in 2023 that scans over 12 million prescription records to spot patterns in generic vs. brand-name outcomes. Early results confirm: no significant difference in interaction rates. The American Medical Association just updated its 2024 guidelines to include specific talking points for doctors: “Your generic drug has the same active ingredient. If you’re having side effects, let’s look at what else changed-your diet, your sleep, your other meds.” And in 2024, the FDA’s “Generics Awareness Campaign” started rolling out nationwide. It’s a $15 million effort to educate patients, pharmacists, and providers about what generics really are-and aren’t. The goal? Reduce the 1.2 million unnecessary brand-name prescriptions filled each year-costing the system $8.7 billion-because people are afraid their generic isn’t working.Bottom Line
Generics don’t interact differently. The active ingredient doesn’t change. The science doesn’t change. But your body might notice the difference in fillers. Your mind might react to the label. Your pharmacy might switch manufacturers without telling you. If you’re on a critical medication like warfarin or levothyroxine, stay consistent. Ask questions. Track changes. Don’t blame the generic. Look at the full picture. And if you’re feeling off? Talk to your pharmacist. They’re the ones who see the labels, the batches, and the patterns. They can tell you if it’s the pill-or something else. You’re not imagining it. But the problem isn’t what you think it is.Are generic drugs less safe than brand-name drugs?
No. Generic drugs are required by the FDA to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must meet the same quality, safety, and effectiveness standards. The FDA approves over 97% of generics based on bioequivalence testing, and post-market surveillance shows adverse event rates are nearly identical between generics and brand-name drugs.
Can inactive ingredients in generics cause side effects?
Yes, but not because they affect how the drug works. Inactive ingredients like lactose, dyes, or preservatives can trigger allergic reactions or intolerances in sensitive individuals. For example, someone with lactose intolerance might feel nauseous after switching to a generic levothyroxine that contains lactose, even though the thyroid hormone itself is unchanged. These are not drug interactions-they’re food sensitivities.
Why do some people say their generic medication doesn’t work as well?
This is often due to the nocebo effect-where expecting a drug to be less effective leads to perceiving side effects or reduced benefit. Studies show patients report more side effects when they know they’re taking a generic, even when the pill is identical to the brand. Other reasons include switching between different generic manufacturers, which changes inactive ingredients, or unrelated factors like diet, stress, or other medications.
Should I stick with the same generic manufacturer?
For drugs with a narrow therapeutic index-like warfarin, levothyroxine, phenytoin, or digoxin-yes. Even small differences in how the body absorbs the drug can lead to dangerous changes in blood levels. The FDA and American Society of Health-System Pharmacists recommend staying with the same generic manufacturer for these drugs to avoid fluctuations. For most other medications, switching is safe.
How can I find out what’s in my generic drug?
Check the packaging or ask your pharmacist for the “inactive ingredients” list. You can also look up the drug by name on the FDA’s Drugs@FDA database or the National Library of Medicine’s DailyMed site. If you have allergies to lactose, gluten, or certain dyes, comparing the ingredients between brand and generic can help you avoid unexpected reactions.
Are generic drugs monitored for safety after they’re approved?
Yes. The FDA requires all drugs-brand and generic-to be monitored through its MedWatch program. Post-marketing surveillance tracks adverse events, including those linked to generic switches. Since 2022, the FDA has updated 17 generic drug labels based on new safety data. The agency also uses AI to analyze millions of real-world prescriptions to detect any unexpected patterns in drug reactions.




December 8, 2025 AT 09:58 AM
so i switched my levothyroxine last month and suddenly felt like a zombie? turns out the new batch had lactose and i didnt even know i was sensitive. my pharmacist was like 'oh yeah, that one's different' and i was like... why didnt u tell me? now i stick with the same brand. no more guessing games.
December 9, 2025 AT 04:05 AM
The notion that generics are 'less effective' is a dangerous myth perpetuated by misinformation and the nocebo effect. The active pharmaceutical ingredient is chemically identical, and the FDA's bioequivalence standards are rigorous. To attribute side effects to the generic itself without ruling out dietary changes, concurrent medications, or psychological factors is scientifically indefensible. Patients deserve accurate information, not fearmongering disguised as personal experience.
December 10, 2025 AT 01:07 AM
im so glad this post exists 😊 i used to think my anxiety was getting worse because my generic sertraline 'wasn't working'... turns out the new version had a different coating that made me nauseous if i took it on an empty stomach. my pharmacist helped me switch back to the one i was on before and boom-my mood stabilized. it's not the drug, it's the little things. thanks for explaining it so clearly 💙
December 11, 2025 AT 19:57 PM
my dad’s on warfarin and they switched his generic twice in six months. his INR went haywire. he didn’t change his diet, didn’t start new meds, didn’t skip doses. just a different pill. he’s back on the same generic now and stable. it’s not about brand vs generic-it’s about consistency. if you’re on a narrow window drug, don’t let your pharmacy play roulette with your health.
December 12, 2025 AT 19:15 PM
Let’s be honest-most people who claim generics don’t work are just too lazy to read the label or too entitled to accept that $4 pills can be just as effective as $40 ones. The FDA doesn’t approve junk. If you’re having side effects, maybe check if you’re eating grapefruit, drinking alcohol, or sleeping five hours a night. Blaming the generic is the lazy person’s excuse for poor health management.
December 14, 2025 AT 14:38 PM
as a nurse who’s seen this over and over, i always tell patients: it’s not the drug, it’s the filler. one lady cried because she thought her antidepressant stopped working-turned out the new generic had red dye #40 and she had a sensitivity. she switched back and felt like herself again. we need more awareness, not more stigma. your body notices things, even if the science says it shouldn’t.
December 14, 2025 AT 20:46 PM
i had a similar experience with phenytoin. switched generics, had a seizure. turned out the new version absorbed slower. my neurologist said it wasn’t the drug-it was the particle size. now i only take the one my pharmacist recommends. i don’t care if it costs $15 more. my brain is worth it.
December 15, 2025 AT 15:07 PM
MY LIFE WAS CHANGED BY THIS POST. I THOUGHT I WAS GOING CRAZY. I WAS ON WARFARIN, SWITCHED GENERICS, STARTED BLEEDING OUT OF MY NOSE. I THOUGHT I WAS DYING. TURNED OUT THE NEW PILLS HAD A DIFFERENT COATING THAT CHANGED ABSORPTION. MY PHARMACIST SAID, 'YOU’RE NOT INSANE, YOU’RE JUST A HUMAN BEING WITH A BODY THAT NOTICES THINGS.' I’M STILL IN SHOCK. THANK YOU. I’M TELLING EVERYONE.