Before 1984, if you needed a generic version of a prescription drug, you were out of luck. There were almost none. The few that existed were expensive to make, legally risky, and took years to get approved. Patients paid full price for brand-name drugs, even after patents expired, because the system didn’t allow competitors to step in. That changed with the Hatch-Waxman Amendments - a law that didn’t just tweak the rules, it rewrote the entire game for how medicines reach American patients.
What the Hatch-Waxman Act Actually Did
The Drug Price Competition and Patent Term Restoration Act of 1984, better known as the Hatch-Waxman Act, was a rare moment of compromise in Washington. Senator Orrin Hatch and Representative Henry Waxman brought together brand-name drug companies and generic manufacturers, two groups that usually hated each other, and got them to agree on something. The result? Two big promises: let generics in faster, and give innovators more time to profit.Before this law, generic companies had to run full clinical trials - the same expensive, multi-year studies that brand-name makers did - just to prove their drug worked. Even if the active ingredient was identical. That made no sense. It was like forcing every bakery to grow its own wheat just to sell bread. Hatch-Waxman ended that. It created the Abbreviated New Drug Application, or ANDA. Now, generic makers only had to prove their drug was bioequivalent - meaning it worked the same way in the body. No need to repeat safety trials. Just show the body absorbs it the same way. That cut development costs by 80-90%.
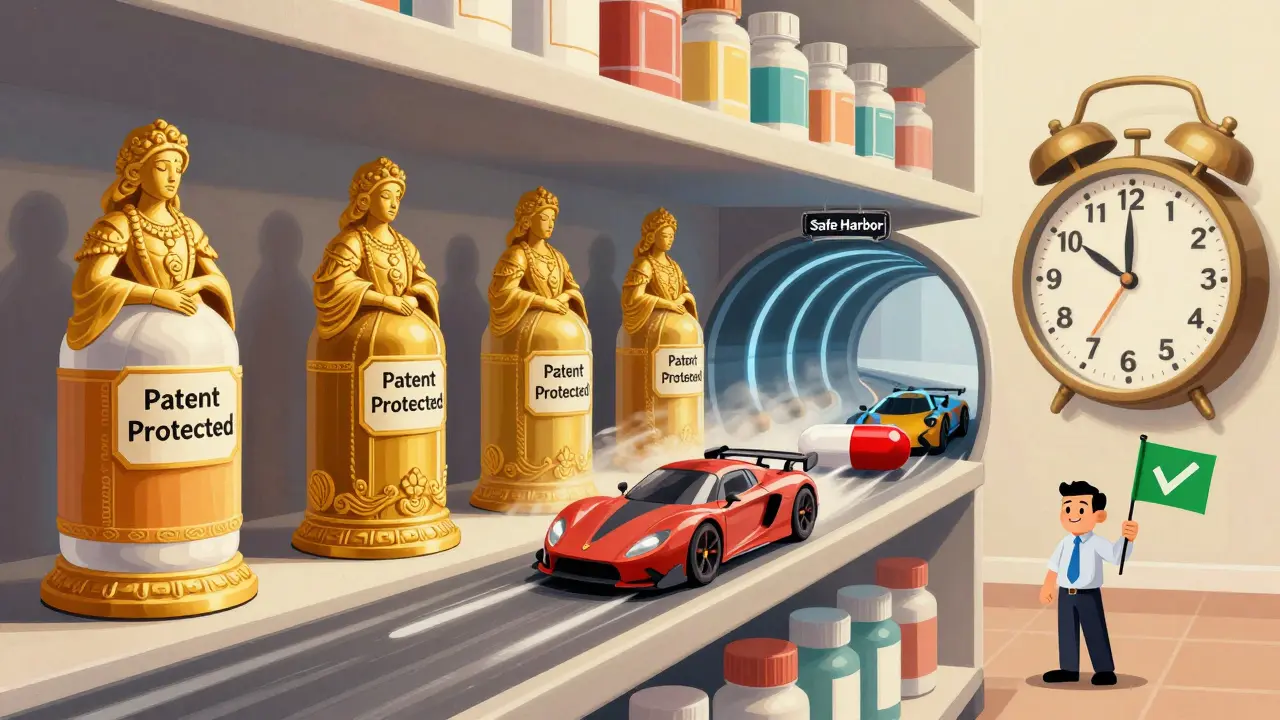
The Patent Game: How Generics Could Challenge Brand Drugs
Here’s where it got clever. The law didn’t just make it easier to copy drugs - it gave generics a legal shield to start the process before the patent expired. Before Hatch-Waxman, a company like Bolar Pharmaceutical got sued just for testing a drug in the lab while the patent was still active. The courts said that was infringement. Hatch-Waxman changed that with something called the “safe harbor” provision. Now, generic companies can legally run tests, even on patented drugs, as long as it’s for FDA approval. No lawsuits. No delays. Just preparation.But here’s the twist: brand-name companies still had patents. So how do generics get past them? The law forced brand-name makers to list every patent related to their drug in the FDA’s Orange Book. When a generic company files an ANDA, it has to say which patent it’s challenging - or say it doesn’t think the patent is valid. That’s called a Paragraph IV certification. And if they do that? They get a huge reward: 180 days of exclusive market access as the first generic to enter. That’s a windfall. One company can make hundreds of millions in those six months before others join.
Why Brand-Name Companies Got Something Too
You can’t just give away the farm. The brand-name companies weren’t going to agree to all this unless they got something back. So Hatch-Waxman gave them patent term restoration. If it took five years for the FDA to approve a new drug, the company could get up to five extra years on its patent clock. That’s not a new patent - it’s an extension. The idea? You spent years waiting for approval. You lost valuable monopoly time. Here’s your compensation.They also got regulatory exclusivity. If a drug was a brand-new chemical, it got five years of market protection - no generics allowed, even if the patent expired. New formulations or uses got three years. Orphan drugs - those for rare diseases - got seven. These weren’t patents. They were legal pauses on competition, built into the system to keep innovation alive.
The Real Impact: 90% of Prescriptions Are Generic Now
The numbers tell the story. In 1983, before Hatch-Waxman, generics made up less than 19% of prescriptions in the U.S. Today? That number is 90%. In 2024, over 10,000 generic drugs were available. They save patients and insurers an estimated $300 billion a year - that’s billions every single month. The average generic costs 80-85% less than the brand-name version. You’re not just saving money. You’re making life-saving drugs accessible to people who couldn’t afford them before.It didn’t happen overnight. The FDA had to build new teams, new systems, new review processes. But by 2022, the average time to approve a generic drug had dropped from 30 months in 2012 to under 12 months. That’s thanks to the Generic Drug User Fee Amendments (GDUFA), which let the FDA charge companies fees to fund faster reviews. It’s a self-sustaining system now.
The Dark Side: Pay-for-Delay and Evergreening
But the system isn’t perfect. The 180-day exclusivity period? It created a gold rush. Some companies filed ANDAs on the exact same day just to race for that window. Others waited for the patent to expire, then filed right away - a tactic called “camping.” The FDA had to step in and say if multiple companies file on the same day, they share the exclusivity. Fairer, but still messy.Then there’s “pay-for-delay.” That’s when a brand-name company pays a generic maker to stay out of the market. Not a lawsuit. Not a patent challenge. Just a check. The FTC found 668 of these deals between 1999 and 2012. They estimated these agreements cost consumers $35 billion a year in higher prices. These deals aren’t illegal - not yet - but they’re the exact opposite of what Hatch-Waxman was meant to do.
And then there’s “evergreening.” That’s when a brand-name company makes a tiny change - a new pill shape, a slightly different dose - and files a new patent. Suddenly, the clock resets. Generics can’t come in. The original patent expired, but now there’s another one. It’s legal. It’s frustrating. And it’s common.

Is the Balance Still Right?
The original law was a compromise. It gave generics a path. It gave innovators a reward. But 40 years later, the world has changed. Drugs cost more. Patents last longer. Big pharma has more tools to delay competition. The FTC and Congress have tried to fix things - like the 2023 Preserve Access to Affordable Generics Act, which wants to ban pay-for-delay deals outright.But here’s the thing: without Hatch-Waxman, we wouldn’t have 90% generic use. We wouldn’t have the billions saved. We wouldn’t have a system that lets a diabetic in rural Ohio afford insulin. The law wasn’t flawless. But it worked - better than anything before it.
Today, the debate isn’t about scrapping it. It’s about fixing its cracks. Can we stop pay-for-delay? Can we limit evergreening? Can we make the 180-day exclusivity fairer? The answer isn’t to go back. It’s to build on what worked.
What Comes Next?
The FDA is still updating its rules. More transparency. Faster reviews. Better tracking of patent challenges. The Generic Drug User Fee Amendments keep getting reauthorized - most recently in 2022 - because the system still needs funding to run efficiently.Meanwhile, patients are watching. When a drug costs $1,000 a month and a generic version could cost $10, people notice. And they ask why it took so long. The answer? It’s not just about science. It’s about law. About incentives. About who gets to play.
Hatch-Waxman didn’t end drug pricing. But it gave the system a heartbeat. And for millions, that heartbeat is the difference between taking a pill - and not.




December 25, 2025 AT 11:36 AM
Man, I remember when my dad couldn’t afford his heart med and had to skip doses. Then generics hit the market and it was like a miracle. No more choosing between groceries and pills. Hatch-Waxman didn’t just change the law-it saved lives.
December 26, 2025 AT 21:15 PM
Let’s be clear: this was regulatory capture disguised as innovation.
December 28, 2025 AT 14:21 PM
Interesting how this law balanced two worlds-profit and access. In India, we’ve seen similar struggles. The cost of insulin used to be a death sentence for families. I wonder if the same model could work elsewhere, especially in low-income countries where patents still block access.
December 29, 2025 AT 04:42 AM
There’s something poetic about a law born from two enemies shaking hands. Hatch and Waxman didn’t care about ideology-they cared about people who couldn’t afford medicine. That’s rare. We’ve forgotten how to compromise in this country. We turn everything into a war. But here? They built a bridge. And millions walk it every day.
December 29, 2025 AT 07:29 AM
Oh please. So now we’re giving gold stars to Big Pharma for letting us buy cheaper pills? Like they didn’t lobby for every loophole in this thing? Pay-for-delay? Evergreening? This law’s a scam dressed in a suit.
December 30, 2025 AT 22:42 PM
The elegance of this legislation lies in its equilibrium. It honored intellectual property while enabling access-a rare triumph of policy over polarization.
January 1, 2026 AT 12:07 PM
wait so the fda charges fees to review generics?? so its like the companies pay to get approved?? that sounds so sketchy??
January 3, 2026 AT 09:42 AM
180 day exclusivity is just corporate welfare disguised as competition
January 4, 2026 AT 19:15 PM
Did you know the FDA was created by shadowy pharmaceutical interests to control the narrative? Hatch-Waxman? A staged performance. The real drug prices are controlled by the Federal Reserve through bond markets. You think insulin is expensive now? Wait till the next currency reset
January 6, 2026 AT 09:26 AM
THIS IS A SETUP. The 180-day exclusivity? That’s not a reward-it’s a bribe. The brand names don’t care if generics come in-they just want to be the ones who get paid to delay them. The whole system is rigged. The FDA? A puppet. Congress? Bought. And you? You’re still paying $400 for a pill that costs $2 to make.
January 7, 2026 AT 20:43 PM
So we reward companies for gaming the system with patent tricks and then call it progress? This isn’t innovation-it’s exploitation. If you want lower prices, ban patents entirely. Don’t give them loopholes and call it a win
January 9, 2026 AT 05:14 AM
Yeah but the 180-day window is wild. One company gets a free pass to charge brand prices for half a year? That’s not competition-that’s a monopoly sandwich. And the brand names? They just wait it out and raise prices again. The whole thing’s a joke.
January 10, 2026 AT 02:04 AM
And yet… we still have people who think this is a free-market triumph? Please. The fact that we need a law to even let generic manufacturers test their own products? That’s not innovation-that’s institutionalized absurdity. The system was designed to fail. And now we’re patting ourselves on the back for fixing it just enough to look decent.
January 11, 2026 AT 03:29 AM
It’s funny how we celebrate this law like it was some heroic act of justice. But behind every generic pill is a lawyer who spent years figuring out how to outmaneuver a patent. The real winners? The firms that hire the best IP attorneys. Not the patients. Not the doctors. The lawyers. That’s the real story.