Kidney Risk Calculator
Assess Your Kidney Risk
Every year, tens of thousands of people end up in the hospital with sudden kidney failure - not from diabetes, not from high blood pressure, but from something many never think twice about: a common painkiller, an antibiotic, or even a heart medication. This isn’t rare. It’s drug-induced kidney injury, and it’s one of the most preventable forms of acute kidney failure you’ve never heard of.
What Exactly Is Drug-Induced Kidney Failure?
Drug-induced kidney injury, or DI-AKI, happens when a medication damages your kidneys so quickly that your body can’t filter waste anymore. It’s not slow, quiet damage like chronic kidney disease. This is a sudden drop in function - sometimes within hours. Your kidneys might stop making urine, or your creatinine levels can spike in days. The result? Hospitalization, dialysis, or even death.
According to the latest data from KDIGO (2024), medications cause about 20% of all acute kidney injury cases in hospitals. In intensive care units, that number jumps to 60%. And here’s the kicker: up to 70% of these cases are preventable. That means most of these kidney failures aren’t accidents - they’re missed opportunities.
How Do Drugs Actually Hurt Your Kidneys?
Not all drugs damage kidneys the same way. There are three main patterns, each with different signs and timing.
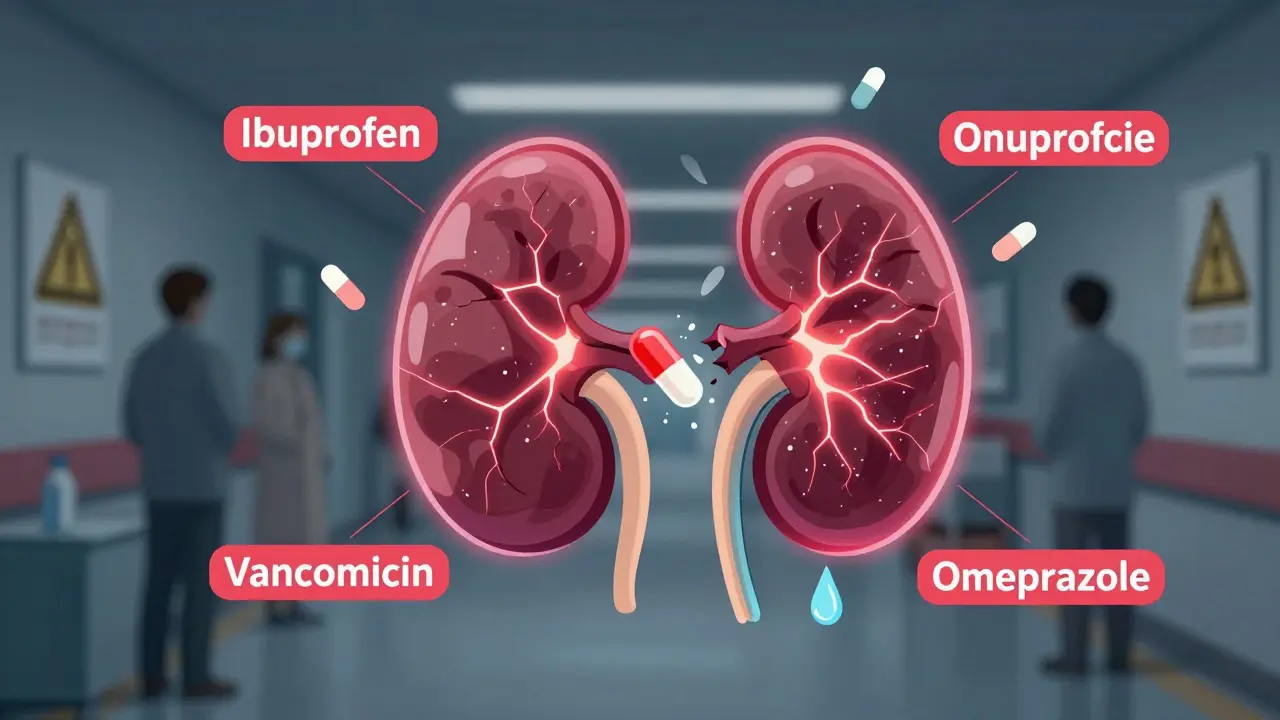
- Acute interstitial nephritis: This is an allergic reaction inside the kidney tissue. It’s often caused by proton pump inhibitors (like omeprazole), antibiotics (especially penicillins and sulfonamides), or NSAIDs. Symptoms don’t show up right away - usually 7 to 14 days after starting the drug. You might get a fever, a rash, or notice your urine looks foamy. Blood tests will show eosinophils climbing. It’s often mistaken for an infection.
- Acute tubular necrosis: This is direct poisoning of the kidney’s filtering tubes. Common culprits are vancomycin, aminoglycosides (like gentamicin), and contrast dyes used in CT scans. It happens fast - within 24 to 72 hours. Your creatinine rises, urine output drops, and you might feel weak or confused.
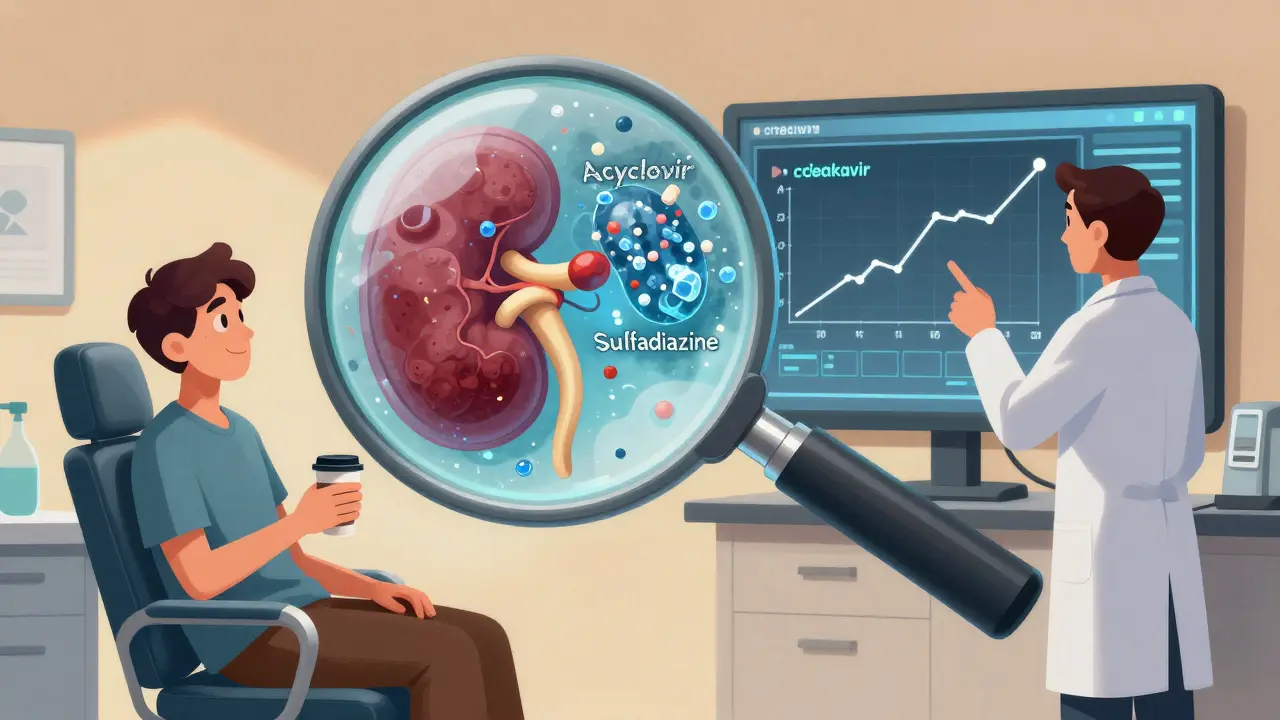
- Crystal-induced nephropathy: Some drugs form crystals in your urine that clog the kidney tubules. Acyclovir (for herpes), sulfadiazine (for infections), and certain HIV drugs like tenofovir can do this. It strikes within hours. The fix? Drink more water and make your urine less acidic. Keeping urine pH above 7.1 can prevent or reverse this damage.
One study of 487 patients found that those with sulfonamide-induced kidney injury who drank 3 liters of water a day and took sodium bicarbonate to alkalize their urine had full recovery - no permanent damage. But those who didn’t? Half ended up with lasting kidney problems.
Who’s at Highest Risk?
You might think only older people or those with known kidney disease are at risk. But that’s not the full picture.
People with an eGFR below 60 mL/min/1.73m² - meaning they already have some kidney impairment - are 3 to 5 times more likely to suffer DI-AKI. But here’s what surprises most doctors: NSAIDs (like ibuprofen, naproxen, celecoxib) are the #1 offender in outpatient settings. They’re sold over the counter, people take them daily for arthritis or back pain, and they’re rarely questioned.
A 2022 study in US Pharmacist found that NSAIDs cause 3-5% of all AKI cases each year. In elderly patients with existing kidney issues? That risk jumps to 15-20%. And it’s not just pills. Topical NSAIDs (gels, patches) can also get absorbed into the bloodstream and harm kidneys - especially in older adults with thin skin or poor circulation.
Polypharmacy is another silent killer. Taking five or more medications at once increases your risk of DI-AKI by nearly four times. Why? Because drugs interact. A blood pressure pill might reduce blood flow to the kidneys. Add an NSAID, and it cuts off what little flow remains. Throw in a diuretic, and you’re dehydrating yourself while your kidneys are already struggling.
How Do You Know It’s Happening?
DI-AKI often flies under the radar. You don’t feel pain in your kidneys. You might just feel “off.” Fatigue. Nausea. Swollen ankles. Less urine. These are easy to dismiss - especially if you’re already sick with something else.
Doctors rely on three key signs:
- A rise in serum creatinine by 0.3 mg/dL or more within 48 hours
- A 50% increase in creatinine from your baseline
- Urine output dropping below 0.5 mL per kg of body weight for 6 hours straight
But here’s the problem: many patients don’t have a baseline creatinine recorded. A 2019 NCEPOD report found that 31% of DI-AKI cases happened because no one checked kidney function before starting a risky drug. That’s like driving blindfolded.
And even when creatinine rises, doctors sometimes delay stopping the drug. One patient, JohnD_72, posted on the American Kidney Fund forum: “I took ibuprofen for 10 days after dental surgery. My creatinine jumped from 1.8 to 4.2 in three days. My doctor didn’t connect the dots for five days. I ended up hospitalized for a week.”
That delay matters. The longer you keep the drug going, the more likely you are to develop permanent scarring. Dr. Mark Perazella from Yale says: “Early recognition and stopping the drug is the single most important step. If you wait too long, you turn acute injury into chronic kidney disease.”
What Medications Are the Biggest Threats?
Not all drugs are equal. Some are more dangerous than others - especially when used long-term or in high doses.
| Drug Class | Examples | Typical Risk Level | Key Prevention Tip |
|---|---|---|---|
| NSAIDs | Ibuprofen, Naproxen, Celecoxib | High | Avoid entirely if eGFR <60. Use acetaminophen instead. |
| Antibiotics | Vancomycin, Piperacillin-tazobactam, Sulfonamides | High | Monitor levels. Hydrate. Avoid in elderly or dehydrated patients. |
| Contrast Dyes | Iodinated contrast for CT scans | Medium-High | Hydrate with saline 6-12 hours before and after. Avoid if eGFR <30. |
| Proton Pump Inhibitors | Omeprazole, Pantoprazole | Medium | Use lowest effective dose. Reassess need every 3-6 months. |
| HIV Medications | Tenofovir, Atazanavir | Medium | Check eGFR before starting. Avoid in patients with eGFR <60. |
The FDA has issued black box warnings for NSAIDs and tenofovir - the strongest possible warning - because of kidney risks. Yet many patients still get these drugs without ever being told about the danger.
How to Prevent It - Real, Proven Strategies
Prevention isn’t complicated. It’s just not done consistently.
Here’s what actually works, based on real-world studies:
- Check kidney function before starting risky drugs. Always. Even if you’re young. A simple blood test for creatinine and eGFR takes 5 minutes. Skip it, and you’re gambling with your kidneys.
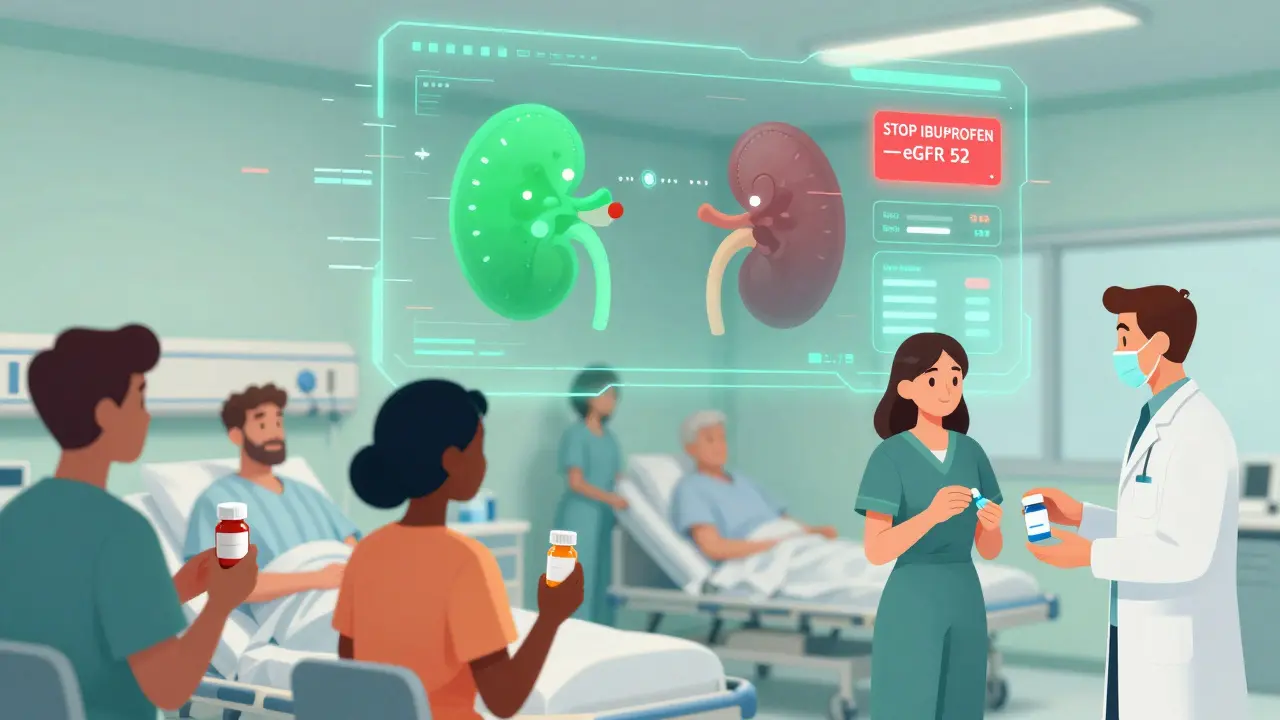
- Stop NSAIDs if your eGFR is below 60. This one change alone can reduce DI-AKI risk by 47%. Use acetaminophen for pain instead. It’s safer for kidneys.
- Use computerized alerts in electronic health records. Hospitals with renal dosing alerts cut inappropriate prescriptions by 63%. If your doctor prescribes a drug that’s risky for your kidney function, the system should flag it.
- Hydrate properly before contrast scans. For high-risk patients (Mehran score ≥16), 1.0-1.5 mL/kg/hour of saline before and after the scan cuts risk by nearly 30%. Sodium bicarbonate? Doesn’t help. Normal saline does.
- For sulfonamides, alkalinize urine. If you’re on sulfadiazine or Bactrim, drink 3+ liters of water daily and ask your doctor about sodium bicarbonate to keep your urine pH above 7.1.
- Do a medication review every 3-6 months. Especially if you’re on five or more drugs. Cut the ones you don’t need. Reduce doses. Simplify. Fewer drugs = less chance of kidney damage.
A 2024 trial of an AI-powered clinical decision tool called Dosis Health showed a 41% drop in DI-AKI cases. Why? Because it didn’t just alert doctors - it told them exactly what to do: “Stop ibuprofen. Check eGFR. Switch to acetaminophen. Hydrate.”
What to Do If You Suspect Kidney Damage
If you’ve been on a new medication and feel unusually tired, have less urine, or notice swelling - don’t wait. Go to your doctor and say: “I think this drug might be hurting my kidneys.”
Ask for:
- A serum creatinine test
- An eGFR calculation
- A urine dipstick to check for protein or blood
- A review of every medication you’re taking
If your creatinine rose more than 0.3 mg/dL in 48 hours, the drug is likely the cause. Stop it immediately - unless your doctor says otherwise. And follow up in 48 hours to see if your numbers are improving.
Remember: kidney damage from drugs is often reversible - if caught early. But if you wait, it can become permanent.
Final Thought: It’s Not Just About the Drug - It’s About the System
One patient, MaryK_65, shared a different story: “My cardiologist switched me from naproxen to acetaminophen after my eGFR dropped to 52. My kidney function stabilized in two weeks.”
That’s what good care looks like. Not luck. Not coincidence. It’s a doctor who checks kidney function, listens to the numbers, and acts.
DI-AKI isn’t inevitable. It’s a system failure. We have the tools. We have the data. We know how to prevent it. What’s missing is consistent action - from doctors, pharmacists, and patients.
Next time you’re prescribed a new pill, ask: “Could this hurt my kidneys?” If the answer isn’t clear, ask for a creatinine test before you start. It’s the simplest, most powerful thing you can do to protect your kidneys.
Can over-the-counter painkillers like ibuprofen really cause kidney failure?
Yes. NSAIDs like ibuprofen and naproxen are among the most common causes of drug-induced kidney injury, especially in people over 65 or those with existing kidney problems. Even short-term use - like taking them for a week after surgery - can cause a sudden drop in kidney function. The risk increases dramatically if you’re dehydrated, taking diuretics, or have an eGFR below 60. Acetaminophen is a safer alternative for most people.
How do I know if my kidneys are already damaged?
You can’t always feel it. The only reliable way is a blood test for creatinine and an eGFR calculation. An eGFR below 60 mL/min/1.73m² means your kidneys aren’t filtering well. A rise in creatinine of 0.3 mg/dL or more in 48 hours is a red flag. If you’re on long-term medications, get tested at least once a year - or before starting any new drug.
Is contrast dye from CT scans dangerous for kidneys?
It can be, especially if your eGFR is below 45. But the risk is preventable. For high-risk patients, doctors should give IV saline before and after the scan. Avoiding contrast entirely isn’t always possible, but hydration and timing make a big difference. Sodium bicarbonate and N-acetylcysteine don’t work as well as plain saline. Always ask your doctor about your risk level before a scan.
Can kidney damage from drugs be reversed?
Often, yes - if caught early. Stopping the drug and staying well-hydrated can allow your kidneys to recover fully within days or weeks. But if the injury continues for more than a few days, scarring can set in, leading to permanent damage. The key is early recognition. Don’t wait for symptoms to get worse.
What should I do if I’m on five or more medications?
Ask for a medication review. Taking five or more drugs increases your risk of kidney injury by nearly four times. Many of these drugs may no longer be necessary, or their doses may be too high for your kidney function. Ask your doctor or pharmacist to go through every pill with you - and challenge the ones that aren’t essential. Simplifying your regimen is one of the best ways to protect your kidneys.
Are there any new tools to help prevent drug-induced kidney injury?
Yes. New AI-powered clinical decision systems, like Dosis Health, are now being used in hospitals to predict and prevent drug-induced kidney injury. These tools analyze your medications, kidney function, and other factors in real time to warn doctors before a harmful prescription is filled. They’ve reduced DI-AKI cases by 41% in clinical trials. If your hospital uses one, ask how it protects your kidneys.
Next Steps: Protect Your Kidneys Today
Here’s what you can do right now:
- Check your latest blood test results. Do you know your eGFR? If not, ask your doctor for it.
- Review your medication list. Are you taking any NSAIDs? If yes, and your eGFR is below 60, talk to your doctor about switching.
- If you’re scheduled for a CT scan with contrast, ask: “What’s my risk? Will I get IV fluids before and after?”
- Set a reminder to get a creatinine test every 6-12 months if you’re over 60 or on chronic medications.
- Keep a list of all your drugs - including supplements and OTCs - and bring it to every appointment.
Your kidneys don’t scream when they’re in trouble. They whisper. You have to listen. And sometimes, the most dangerous thing you’re taking isn’t a prescription - it’s the one you bought without a thought at the pharmacy counter.




January 15, 2026 AT 11:16 AM
NSAIDs are just poison wrapped in a pill. People take them like candy and wonder why they end up on dialysis. Stop the madness.
January 15, 2026 AT 14:24 PM
It's truly disheartening to see how casually society treats medications as harmless conveniences. The fact that over-the-counter NSAIDs are responsible for such a staggering percentage of preventable kidney injuries speaks volumes about our collective disregard for basic physiological boundaries. We've normalized risk to the point where a simple blood test is considered an inconvenience rather than a necessity.
January 17, 2026 AT 08:42 AM
You're not alone if you've been taking ibuprofen for years without knowing the risks. But here's the good news: it's never too late to make a change. Switch to acetaminophen, drink more water, and talk to your doctor. Your kidneys will thank you. You got this!
January 18, 2026 AT 13:49 PM
They say 70% of cases are preventable. That's because the system is rigged. Big Pharma doesn't want you to know that your painkiller is slowly killing your kidneys. They'd rather you take it daily and need more drugs later. Wake up.
January 20, 2026 AT 07:54 AM
i got a ct scan last year and they didnt even ask if i was on meds. just handed me the form and said 'drink this'. dumb.
January 20, 2026 AT 17:25 PM
The real tragedy isn't the nephrotoxicity-it's the epistemological laziness of modern medicine. We reduce complex physiological systems to binary risk tables while ignoring the phenomenological experience of the patient. The algorithm doesn't see your dehydration, your anxiety, your sleep-deprived state-it sees a number. And that number becomes your verdict.
January 21, 2026 AT 07:23 AM
i used to take ibuprofen for everything until my cousin got hospitalized after a weekend of back pain meds. now i just stretch and ice it. simple works better than pills anyway
January 22, 2026 AT 11:09 AM
They call it drug-induced kidney injury like it's some freak accident. Nah. It's the logical endpoint of a culture that treats the body like a machine you can keep running on cheap fuel. You don't pour diesel into a gasoline engine. Why do we think we can pour NSAIDs into our kidneys and expect them to hold up?
January 23, 2026 AT 06:25 AM
I would like to emphasize the critical importance of baseline renal function assessment prior to initiating any nephrotoxic agent. This is not merely a clinical recommendation-it is a standard of care. Failure to obtain an eGFR before prescribing NSAIDs or contrast agents constitutes a breach in the duty of care, and institutions must be held accountable.
January 23, 2026 AT 21:29 PM
It's wild how something so simple-like asking 'Could this hurt my kidneys?'-can save so much suffering. We're taught to trust doctors, but we're never taught to ask questions. Maybe the real medicine isn't in the pill, but in the conversation you have before you take it.
January 25, 2026 AT 08:13 AM
Oh, so now we're blaming the patient for not reading the 47-page FDA warning buried in the tiny print on the bottle? Let me guess-your doctor also told you to 'drink more water' while prescribing you ten different drugs that dehydrate you. How quaint. The system isn't broken-it's designed this way.
January 25, 2026 AT 13:38 PM
AI tools like Dosis Health? That’s just the next step in corporate surveillance. They’re not protecting your kidneys-they’re collecting your data to sell to insurers. Next thing you know, your insurance will deny you NSAIDs because your 'risk profile' says you're 'likely to develop kidney injury.' And guess who pays? You. Always you.