Delayed Reaction Symptom Checker
Your Symptoms
Select your symptoms above and click "Check My Symptoms" to see if they might indicate a delayed medication reaction.
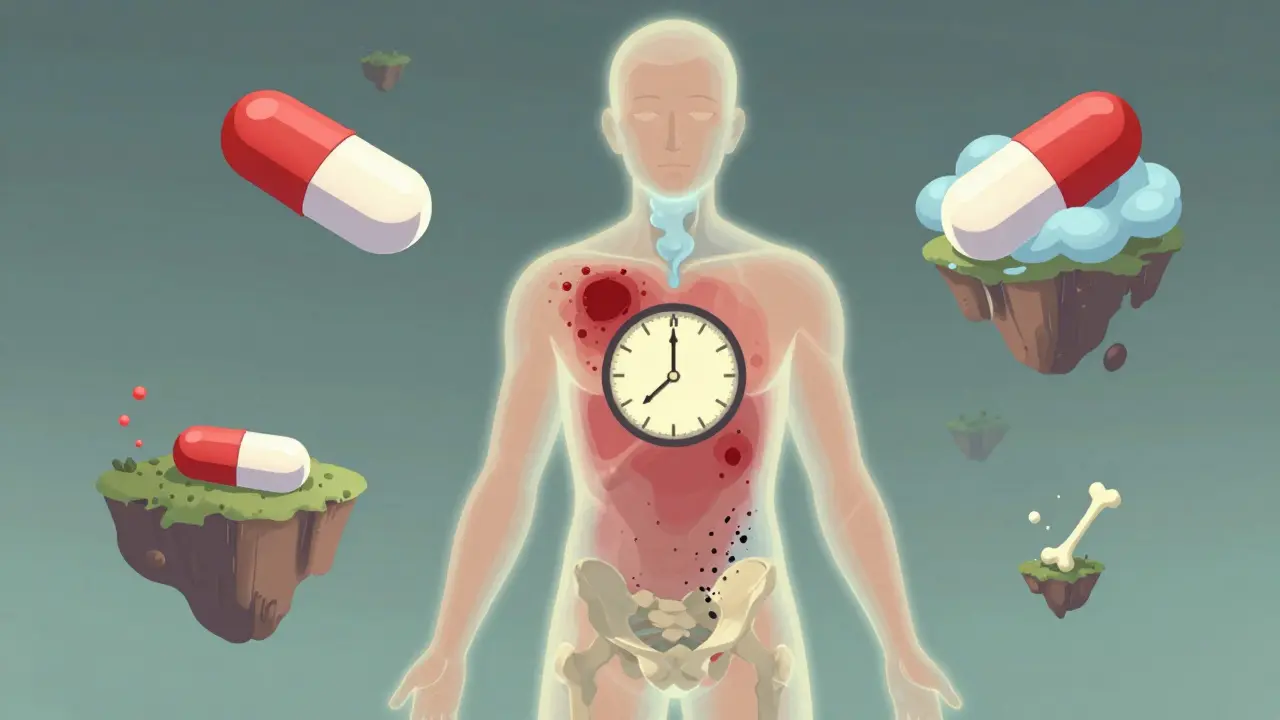
Why Your Medication Might Start Hurting You Months Later
You’ve been taking your pill for years. No problems. No rashes, no dizziness, no strange swelling. Then, out of nowhere, your skin breaks out in angry red patches. Or your tongue swells shut at 3 a.m. Or your joints ache like you’ve run a marathon every day for a month. You didn’t change your diet. You didn’t start a new workout. You didn’t catch a virus. But your body is screaming something’s wrong. Here’s the hard truth: delayed medication side effects don’t care how long you’ve been safe. They can wait. They can hide. And when they finally show up, doctors often miss them. This isn’t rare. In fact, about one in every 20 hospital admissions in the U.S. and Europe is linked to a bad reaction to a drug. And nearly a third of those? They didn’t show up until days, weeks, or even years after you started the medicine. You might think, “But my doctor said this was safe.” And they believed it. Most of the time, they’re right-at first. But drugs don’t always behave the way they do in clinical trials. Real people live for decades. Their bodies change. Their genetics speak up. And sometimes, the reaction is slow, sneaky, and deadly.What Exactly Is a Delayed Reaction?
A delayed reaction isn’t just a side effect that shows up late. It’s a specific kind of biological betrayal. Your immune system, which normally protects you, starts attacking your own tissues because it got confused by a drug. The classic example? ACE inhibitors like lisinopril or enalapril. People take them for high blood pressure for 5, 10, even 20 years. Then, one day, their face swells. Their throat tightens. They can’t breathe. Emergency teams rush in. The patient says, “I’ve been on this for years-how is this happening?” The answer: delayed hypersensitivity. It’s not an allergy like peanut or bee venom. It’s a Type IV reaction, named after Coombs and Gell’s 1960s classification system. These reactions don’t spike within minutes. They simmer. They build. They can take 48 hours to 8 weeks to fully erupt. And it’s not just skin deep. These reactions can wreck your liver, kidneys, lungs, even your bone marrow. DRESS syndrome-Drug Reaction with Eosinophilia and Systemic Symptoms-is one of the most dangerous. It starts with a rash, then fever, swollen lymph nodes, and organ failure. Mortality? Up to 10%. And it usually hits 2 to 8 weeks after you start the drug.Which Drugs Are Most Likely to Cause Delayed Reactions?
Some medications are quietly dangerous over time. Here’s who’s on the list:- Fluoroquinolone antibiotics (ciprofloxacin, levofloxacin): These are linked to tendon ruptures-even months after you finish the course. The FDA added black box warnings in 2018 after over 1,000 reports of people tearing their Achilles tendons after taking these for a simple sinus infection.
- Proton pump inhibitors (omeprazole, esomeprazole): Used for heartburn. Safe, right? Not if you take them for more than two years. Your body stops absorbing vitamin B12, magnesium, and calcium. Risk of fractures? Up 30%. Risk of kidney damage? Doubles after four years.
- Corticosteroids (prednisone): Great for inflammation. Terrible for your bones. After 12+ months, osteoporosis kicks in. So do cataracts and diabetes. You might not notice until you break a hip from a simple fall.
- Metformin: The go-to for type 2 diabetes. But after four years, up to 30% of users develop vitamin B12 deficiency. Symptoms? Numbness, fatigue, memory fog. Often mistaken for aging or neuropathy.
- Antiepileptics (carbamazepine, phenytoin): Can trigger Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis-burning, blistering skin that peels off like a sunburn. Mortality? Up to 50% in the worst cases. Genetic testing can catch this before it starts.
- Allopurinol: Used for gout. Can cause DRESS. Especially dangerous if you’re Asian and carry the HLA-B*58:01 gene variant.

Who’s Most at Risk?
Not everyone gets hit the same way. Some people are walking time bombs.- People over 65: They make up only 16% of the population but account for 25% of all emergency visits for drug reactions. Why? Slower metabolism. Multiple meds. Weaker immune systems.
- Women: Studies show women have 1.5 to 2 times higher risk of delayed hypersensitivity. Hormones likely play a role.
- People with autoimmune diseases: If you have Crohn’s, lupus, or rheumatoid arthritis, your immune system is already on edge. Taking thiopurines or biologics? Your risk of DRESS skyrockets-up to 12 times higher.
- Those with certain genes: HLA-B*15:02? Avoid carbamazepine. HLA-B*57:01? Don’t take abacavir for HIV. These aren’t guesses. They’re genetic red flags. Screening exists. But most doctors don’t order it unless you’re in a specialized clinic.
How Do You Know It’s the Drug-and Not Something Else?
This is the biggest trap. Doctors look for infections. Autoimmune flares. Cancer. Rare diseases. They rarely think: “Could this be a drug I prescribed three months ago?” Here’s how to spot a delayed reaction:- Did symptoms start after you began a new medication, even if it was weeks or months ago?
- Are you experiencing multiple symptoms at once? Rash + fever + swollen glands + liver enzymes up? That’s a red flag.
- Did you feel fine for months-or years-then suddenly crash?
- Are your symptoms improving after stopping the drug? That’s the strongest clue.

What Should You Do If You Suspect a Delayed Reaction?
1. Stop the drug immediately-but only if you can. Don’t quit blood pressure meds or seizure meds without talking to your doctor. Some reactions get worse if you stop cold turkey. 2. Write down everything: When did you start the drug? When did symptoms begin? What’s changed? List every pill, supplement, and herbal product. 3. See a specialist: A dermatologist can do a skin biopsy. An allergist can run lymphocyte transformation tests (85% accurate for delayed reactions). A pharmacologist can map your drug history. 4. Report it: File a report with your country’s drug safety agency (FDA’s FAERS in the U.S., TGA in Australia). These reports save lives. They trigger warnings, label changes, and research. 5. Get genetic testing if recommended: If you’re prescribed carbamazepine, allopurinol, or abacavir, ask if you’ve been tested for HLA variants. It’s a simple blood test. Could save your life.What’s Changing in 2026?
We’re finally catching up. The FDA’s Sentinel Initiative now tracks over 200 million patient records using AI to predict who’s at risk for delayed reactions before they even get the prescription. By 2025, hospitals in the U.S. and Europe will routinely screen for key genetic markers before prescribing high-risk drugs. In Australia, the Therapeutic Goods Administration (TGA) updated labeling for fluoroquinolones in January 2024 to include stronger warnings about tendon damage up to six months after use. PPIs now carry a mandatory note about B12 and magnesium deficiency after two years. And patients? We’re getting louder. On Reddit, HealthUnlocked, and Drugs.com, thousands have shared stories of being ignored-until they weren’t. One woman in Sydney told me her story: “I had a rash for six weeks. My GP said it was stress. My dermatologist said it was eczema. I finally asked about the lisinopril. They stopped it. The rash vanished in 72 hours.”Don’t Wait for a Crisis
Medications aren’t harmless. They’re powerful tools-and like any tool, they can turn on you if you don’t pay attention. If you’ve been on the same pills for years, take 10 minutes this week to review them. Ask yourself: - Has anything changed in my body lately? - Did I start any new drug-even a low-dose one-within the last 6 months? - Could any of my symptoms be linked to a pill I’ve been taking for years? Write it down. Bring it to your next appointment. Don’t let silence be your doctor’s default answer. Delayed reactions don’t announce themselves. But they’re not invisible. You just have to know what to look for.Can delayed side effects happen after years of taking a medication safely?
Yes. Many delayed reactions occur after months or even years of uneventful use. For example, ACE inhibitors like lisinopril can cause angioedema after 7-10 years of safe use. Proton pump inhibitors may lead to vitamin B12 deficiency or kidney damage after 2-4 years. The body’s response can change over time due to aging, genetics, or interactions with other medications.
What are the most common symptoms of a delayed drug reaction?
The most common signs include unexplained skin rashes (especially widespread or blistering), fever, swollen lymph nodes, joint pain, fatigue, and organ-specific symptoms like jaundice (liver), reduced urine output (kidneys), or shortness of breath (lungs). Neurological symptoms like slurred speech, tremors, or numbness can also appear due to nutrient deficiencies caused by long-term drug use.
How long after starting a drug can a delayed reaction appear?
Timing varies by reaction type. Type IV hypersensitivity (like DRESS or contact dermatitis) usually appears 2-8 weeks after starting the drug. Tendon damage from fluoroquinolones can show up 1-6 months after finishing the course. Conditions like osteoporosis from steroids or B12 deficiency from metformin may take 1-4 years to become noticeable.
Are delayed reactions more common in older adults?
Yes. Adults over 65 account for about 25% of all emergency visits for drug reactions, even though they make up only 16% of the population. This is due to slower drug metabolism, multiple prescriptions, and age-related changes in liver and kidney function that increase drug accumulation and immune sensitivity.
Can genetic testing help prevent delayed reactions?
Absolutely. Genetic screening for HLA-B*15:02 before prescribing carbamazepine reduces the risk of Stevens-Johnson Syndrome from 50-80% to near zero in carriers. Similarly, testing for HLA-B*57:01 prevents abacavir hypersensitivity. These tests are simple, affordable, and increasingly recommended before prescribing high-risk drugs.
What should I do if I think a medication is causing a delayed reaction?
Don’t stop critical medications without medical advice. Instead, document your symptoms and timeline, list all medications you’re taking, and consult a specialist-ideally an allergist, dermatologist, or clinical pharmacologist. Request a lymphocyte transformation test or skin patch test if appropriate. Report the reaction to your national drug safety agency to help others.
Can delayed reactions be reversed?
Many can be, if caught early. Stopping the drug often leads to full recovery-especially for rashes, fever, or mild organ dysfunction. But some damage, like tendon rupture from fluoroquinolones or permanent kidney injury from PPIs, may be irreversible. Early recognition is key to preventing long-term harm.



February 3, 2026 AT 18:41 PM
So let me get this straight-your doctor prescribes you a pill for 10 years, and then one day your face swells up like you’ve been kissed by a angry bee? And they act like it’s a surprise? 🤦♂️ We’ve known about DRESS syndrome since the 90s. The FDA’s been dragging their feet. This isn’t science, it’s corporate negligence wrapped in a white coat.
February 5, 2026 AT 15:03 PM
omg i had this exact thing with lisinopril 😭 i thought it was just my allergies getting worse... then i read this and was like WAIT. i stopped it and my lips went back to normal in 3 days. why do docs not tell us this stuff?? 🇨🇦 we need better med safety here too
February 6, 2026 AT 02:50 AM
i been on metformin for 5 years and lately my hands go numb like im holding ice cubes i thought it was carpal tunnel but now im wondering if its the b12 thing they mentioned here
February 7, 2026 AT 13:58 PM
Just a quick note-lymphocyte transformation tests aren’t available everywhere, even in the UK. My rheumatologist had to refer me to a specialist lab in London. If you suspect a delayed reaction, ask for a referral to a clinical pharmacology unit. They’re rare but lifesavers. Also, report it to the Yellow Card scheme. Every report counts. 🙏
February 9, 2026 AT 00:47 AM
I used to work in a pharmacy. Saw this over and over. Elderly patients on 7 meds, all ‘safe’ according to the chart. Then boom-kidney crash, or weird rash, or ‘sudden dementia’ that was just B12 deficiency from PPIs. Doctors don’t have time to connect the dots. Patients need to be their own advocates. It’s not paranoia. It’s survival.
February 10, 2026 AT 19:51 PM
The pharmacokinetic and pharmacodynamic variability in aging populations is well-documented in the literature. Polypharmacy increases the likelihood of non-linear metabolic interactions, particularly with cytochrome P450 substrates. The delayed hypersensitivity mechanisms, particularly Type IV T-cell mediated responses, are under-recognized in primary care due to diagnostic latency and lack of standardized screening protocols.
February 11, 2026 AT 10:57 AM
This hit me right in the soul 🥺 I’ve been on prednisone for 18 months for my lupus. Last month I broke my wrist picking up my coffee mug. I thought I was just clumsy. Turns out my bones are basically chalk. I cried for an hour. But now I’m asking for a DEXA scan. Thank you for writing this. We need more voices like yours. 🙏❤️
February 12, 2026 AT 16:36 PM
i am from india and my uncle had allopurinol reaction... he got dres and almost died. we were lucky we found out fast. i think genetic testing should be free or cheap for everyone. why make people suffer because they cant afford a blood test? 🤔
February 13, 2026 AT 13:56 PM
So we’re just supposed to live in fear of every pill we take? What’s next? Will we need a background check on our liver before getting a prescription? The system is broken. We’re not patients. We’re data points with a pulse.