When someone is trying to quit drinking, the right medication can make all the difference. Antabuse (disulfiram) has been around since the 1940s and works by making alcohol consumption deeply unpleasant-nausea, vomiting, flushing, and rapid heartbeat kick in within minutes. But while it’s effective for some, it’s not for everyone. Side effects can be harsh, interactions with other medications are risky, and forgetting to take it means the deterrent vanishes. That’s why many doctors and patients are turning to Antabuse competitor drugs that work differently-and often more safely.
Why People Look for Antabuse Alternatives
Antabuse isn’t a cure. It’s a deterrent. You still have to want to stop drinking. If you miss a dose, the protection disappears. Some people can’t tolerate the side effects. Others are on medications that react dangerously with disulfiram, like certain antidepressants or seizure drugs. And then there’s the psychological burden: living with the fear of accidental exposure to alcohol-like in mouthwash, sauces, or even hand sanitizer-can be exhausting.
That’s where newer options come in. They don’t rely on punishment. Instead, they target the brain’s reward system, reduce cravings, or ease withdrawal symptoms. They’re often easier to stick with, have fewer drug interactions, and don’t require strict daily discipline to work.
Top Antabuse Competitor Drugs in 2025
Three FDA-approved medications are now the most common alternatives to Antabuse. Each works in a different way, and choosing the right one depends on your medical history, drinking patterns, and personal goals.
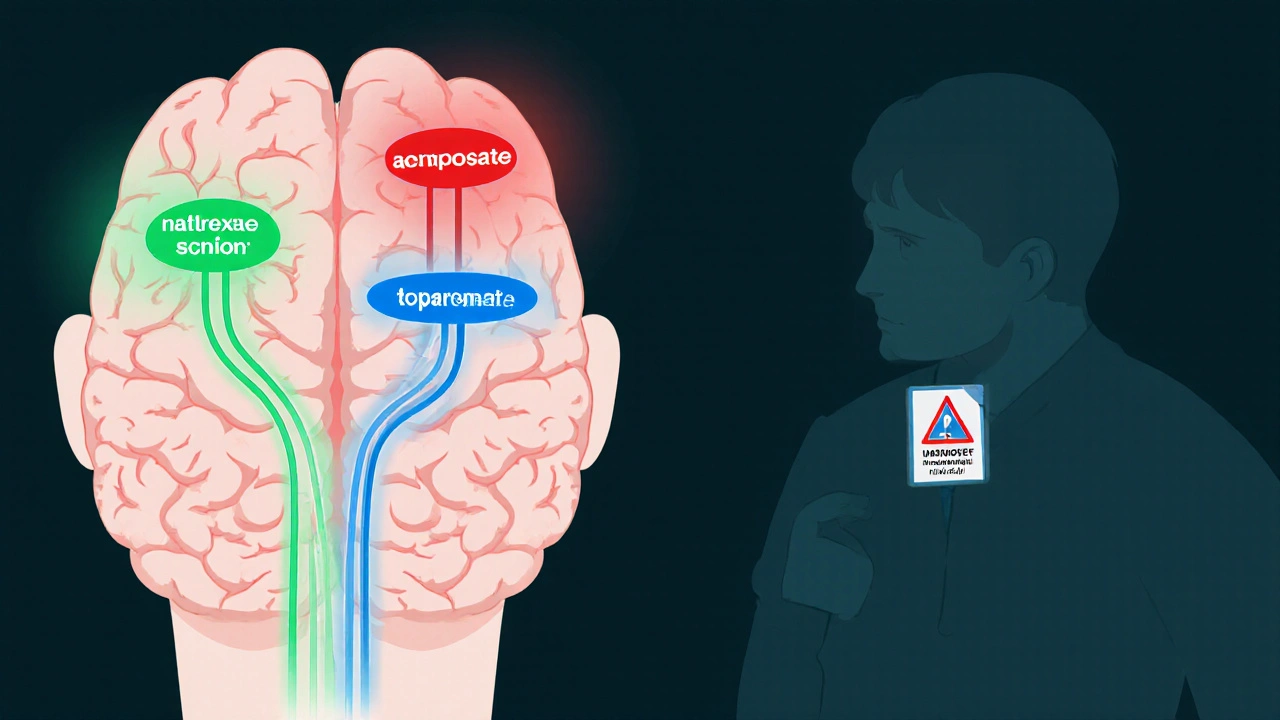
Naltrexone (Vivitrol, Revia)
Naltrexone blocks opioid receptors in the brain. Alcohol triggers the release of endorphins, which make drinking feel rewarding. Naltrexone cuts that pleasure signal. Over time, drinking becomes less appealing. It doesn’t make you sick if you drink-it just makes it less satisfying.
Available as a daily pill (Revia) or a monthly injection (Vivitrol), it’s ideal for people who want to reduce heavy drinking or stop entirely. Studies show it cuts relapse rates by about 25% compared to placebo. The injection version eliminates the need for daily pills, which helps with adherence. Side effects are mild: nausea, headache, or dizziness in the first week. It’s safe for people with liver disease, unlike Antabuse.
Acamprosate (Campral)
Acamprosate doesn’t touch pleasure. It targets the brain’s stress response after quitting. Heavy drinking disrupts the balance between excitatory and calming brain chemicals. When you stop, your brain goes into overdrive-leading to anxiety, insomnia, restlessness, and cravings. Acamprosate helps restore that balance.
It’s taken three times a day and works best after you’ve already stopped drinking. It’s not for people still drinking daily. Clinical trials show it increases the chance of staying sober for at least six months by 15-20%. It’s gentle on the liver and kidneys, making it a top choice for older adults or those with chronic health conditions.
Topiramate (Topamax)
While not FDA-approved specifically for alcohol use disorder, topiramate is widely used off-label and backed by solid research. Originally an anti-seizure and migraine drug, it reduces cravings by modulating GABA and glutamate-two key neurotransmitters involved in addiction.
Studies from the National Institute on Alcohol Abuse and Alcoholism show topiramate can reduce heavy drinking days by up to 50% in some patients. It’s often prescribed when naltrexone and acamprosate haven’t worked. Side effects include tingling in hands and feet, memory issues, or taste changes (carbonated drinks taste flat). Most people adjust within a few weeks. Dosing starts low and increases slowly.
How These Drugs Compare to Antabuse
Here’s how the main alternatives stack up against disulfiram:
| Medication | How It Works | Form | Best For | Common Side Effects | Alcohol Interaction |
|---|---|---|---|---|---|
| Antabuse (disulfiram) | Causes severe reaction to alcohol | Daily pill | Highly motivated, stable patients | Headache, fatigue, metallic taste, liver strain | Severe: nausea, vomiting, chest pain, low blood pressure |
| Naltrexone | Blocks alcohol’s rewarding effects | Pill or monthly injection | Reducing heavy drinking, preventing relapse | Nausea, headache, dizziness | No reaction-just less pleasure |
| Acamprosate | Stabilizes brain chemistry after quitting | Three times daily pill | Early sobriety, anxiety, insomnia | Diarrhea, gas, depression | No reaction |
| Topiramate | Reduces cravings via GABA/glutamate | Daily pill | When other meds fail | Tingling, memory issues, taste changes | No reaction |
One key difference: Antabuse is a behavioral deterrent. The others are neurochemical tools. You don’t need to fear alcohol with naltrexone or acamprosate-you just feel less drawn to it. That’s a big shift in mindset for many people.

What About Newer Options?
Research is moving fast. In 2024, the FDA granted fast-track status to a new drug called cenobamate, which shows promise in reducing alcohol cravings with fewer cognitive side effects than topiramate. Early trials suggest it may help people who’ve failed other treatments.
There’s also growing interest in psilocybin-assisted therapy for alcohol use disorder. A 2023 Johns Hopkins study found that two doses of psilocybin, combined with counseling, led to 80% of participants abstaining from alcohol for six months-double the rate of standard therapy. While not yet approved as a medication, it’s being studied in clinical trials across the U.S. and Australia.
For now, though, naltrexone, acamprosate, and topiramate remain the most accessible, evidence-backed options. If you’re looking for a safer, more sustainable path than Antabuse, these are your best starting points.
For a full breakdown of current options, including dosing guidelines and insurance coverage, see this detailed guide on Antabuse competitor drugs.
How to Choose the Right One
There’s no one-size-fits-all. Your doctor will consider:
- How much you’ve been drinking (daily heavy use vs. occasional bingeing)
- Your medical history (liver health, mental health, other medications)
- Your lifestyle (can you take pills three times a day? Or do you need a monthly shot?)
- Your goals (total abstinence or cutting back?)
Many people start with naltrexone because it’s flexible. If cravings persist, they add acamprosate. Topiramate is usually a second-line option. Antabuse is often reserved for those who’ve tried everything else and are ready for a strict, high-stakes approach.

What Doesn’t Work
Some people try herbal supplements like kudzu, milk thistle, or ibogaine. There’s no strong evidence they work for alcohol dependence. Others rely on willpower alone-which works for some, but fails for most. Medication-assisted treatment (MAT) is the gold standard for a reason: it combines science with support.
Also avoid mixing any of these drugs with alcohol, even in small amounts. While naltrexone and acamprosate won’t cause a reaction, they’re designed to help you stay away from alcohol entirely. Taking them while drinking defeats the purpose.
Real Stories, Real Results
One patient in Melbourne, 52, had been on Antabuse for eight months. He’d stopped drinking but lived in constant fear of accidental exposure. He switched to naltrexone after his doctor explained how it worked. Within weeks, he stopped checking ingredient labels on sauces and started going to restaurants again. He says, “I didn’t feel punished anymore. I just didn’t want to drink.”
A nurse in Perth, 38, struggled with anxiety after quitting. Acamprosate calmed her nerves and helped her sleep. She’s been sober for 14 months. “It didn’t make me feel good,” she says. “But it stopped me from feeling awful.”
Next Steps
If you’re considering alternatives to Antabuse, talk to your doctor or an addiction specialist. Bring a list of your current medications and your drinking history. Ask about naltrexone or acamprosate first-they’re safer, easier to use, and just as effective for most people.
Don’t assume Antabuse is your only option. The landscape has changed. There are now multiple ways to treat alcohol dependence without fear, punishment, or daily dread.
Is Antabuse still used today?
Yes, but less often. Antabuse is still prescribed, especially for patients who respond well to behavioral deterrents and have strong support systems. However, most doctors now prefer naltrexone or acamprosate because they’re safer, easier to take, and don’t carry the risk of dangerous reactions.
Can I switch from Antabuse to naltrexone?
Yes, but you must stop Antabuse for at least 14 days before starting naltrexone. Disulfiram stays in your system for up to two weeks. Starting naltrexone too soon can reduce its effectiveness. Always consult your doctor before switching.
Do any of these drugs cause weight gain?
Naltrexone and acamprosate rarely cause weight gain. In fact, some people lose weight after quitting alcohol. Topiramate can suppress appetite and may lead to modest weight loss. Antabuse doesn’t directly cause weight gain, but some people gain weight after quitting drinking due to increased food intake.
Are these medications covered by insurance?
In Australia, naltrexone and acamprosate are listed on the PBS (Pharmaceutical Benefits Scheme), meaning they’re heavily subsidized. Topiramate is covered for epilepsy and migraines, but off-label use for alcohol dependence may require prior authorization. In the U.S., coverage varies by plan, but most major insurers cover these medications for alcohol use disorder.
How long do I need to take these drugs?
Most people take them for at least six months to a year. Some stay on them for years, especially if they’ve had multiple relapses. Unlike antibiotics, these aren’t meant to be taken for a short time. Think of them like blood pressure medication-long-term use prevents relapse. Stopping too early increases the risk of returning to heavy drinking.



November 19, 2025 AT 21:03 PM
This is the most useful thread I've seen on this topic in years. Seriously, if you're still on Antabuse, just switch already.
November 20, 2025 AT 19:30 PM
Naltrexone changed my life 😊 I used to check every sauce label like it was a bomb threat. Now I eat at Thai places again. No more panic. Just peace. 🙏
November 20, 2025 AT 22:07 PM
topiramate is just a brain fog machine. i took it for 3 wks and forgot my own name. not worth it.
November 22, 2025 AT 10:17 AM
Of course the FDA approves these 'safer' drugs... while the real solution-abstinence and willpower-is ignored. Big Pharma doesn't want you cured, they want you dependent on pills forever. Wake up.
November 23, 2025 AT 16:51 PM
Why are we letting Western medicine dictate how Africans and Indians should treat addiction? We had traditional remedies for centuries before these chemical cages came along
November 23, 2025 AT 20:52 PM
I appreciate how this post breaks it down without judgment. I was on Antabuse for 11 months and it felt like living with a time bomb in my pocket. Switching to acamprosate was like finally breathing again. I didn’t need to fear my own kitchen. The brain chemistry stuff? It’s real. It’s not magic, but it’s not punishment either. It’s repair. And honestly? That’s way more dignified than being scared into sobriety. I used to avoid birthday parties because of the wine in the punch. Now I go. I don’t drink. But I’m not terrified either. That’s the difference between a deterrent and a tool. One makes you feel like a criminal. The other makes you feel like a human trying to heal.
November 25, 2025 AT 19:53 PM
Let’s not forget the elephant in the room: adherence. Antabuse fails because humans forget. Naltrexone injection? One shot a month. Acamprosate? Three pills, you can tie it to coffee. Topiramate? Slow titration, less brain fog than people say. The real win isn’t the mechanism-it’s the fact that these options respect your autonomy. You’re not being punished; you’re being supported. And psilocybin? Don’t sleep on it. Johns Hopkins data is solid. It’s not a drug, it’s a reset button for the brain’s reward pathways. We’re not talking hippie vibes here-we’re talking fMRI scans showing neural rewiring. This isn’t the 90s anymore. Treatment is evolving. Get with it.
November 26, 2025 AT 08:12 AM
Of course they're pushing these 'gentler' drugs-they're more profitable. Antabuse is cheap, generic, and requires zero follow-up. These new meds? Monthly shots. Three-times-daily pills. Insurance billing codes. The system doesn't care if you're sober-it cares if you're paying monthly. Wake up. This isn't medicine. It's a subscription model.
November 27, 2025 AT 09:55 AM
How ironic that we’ve replaced one form of psychological torture (Antabuse) with another: the illusion of choice. Naltrexone doesn’t cure craving-it just dulls it. Acamprosate doesn’t heal trauma-it masks anxiety. We’re medicating symptoms while ignoring root causes: childhood neglect, systemic poverty, the crushing weight of modern alienation. You think a pill fixes that? Please. These drugs are Band-Aids on a hemorrhage. And psilocybin? A spiritual placebo for the overeducated. Real recovery isn’t chemical-it’s communal. It’s accountability. It’s a village. Not a pharmacy.
November 27, 2025 AT 14:49 PM
...And yet, not one of these studies accounts for the placebo effect of pharmaceutical branding. Naltrexone’s efficacy? Correlated with patient expectations. Vivitrol’s ‘monthly injection’? A psychological crutch. The real variable isn’t the drug-it’s the patient’s belief in the ritual. Antabuse’s horror-story mechanism? That’s the placebo in reverse: fear as a therapeutic agent. The data is noise. The truth? Addiction is behavioral. And behavior? It’s changed by consequence. Not chemistry.
November 29, 2025 AT 07:12 AM
Wow. So we’ve replaced ‘drink and die’ with ‘drink and feel blah.’ Progress? Or just a more expensive form of denial?
November 30, 2025 AT 17:31 PM
While the pharmacological distinctions are well-articulated, one must consider the socio-economic accessibility of these alternatives. In rural America, the monthly Vivitrol injection requires transportation, clinic access, and insurance pre-authorization-a non-trivial barrier. Meanwhile, disulfiram, though hazardous, is available in generic form at $5 per month. The narrative of ‘safer’ alternatives may inadvertently marginalize those least equipped to navigate complex healthcare systems. One wonders whether the shift is clinically superior, or merely aesthetically preferable to clinicians.
December 2, 2025 AT 15:16 PM
My cousin in Texas switched from Antabuse to naltrexone. He said it felt like the weight of a thousand invisible eyes lifted. He didn’t feel like a bad person anymore. Just someone trying. That’s worth more than any side effect chart.
December 3, 2025 AT 17:19 PM
just wanted to say i’ve been on acamprosate for 18 months now and honestly? it’s not magic but it’s the reason i’m still here. i had panic attacks every night after quitting. this stuff didn’t make me happy… but it stopped me from feeling like i was falling apart. if you’re scared to try it, just talk to your doc. you don’t have to do this alone. you got this 💪