Every year in the U.S., more than 1.5 million people end up in the emergency room because of something gone wrong with their medication. That’s not a typo. It’s not rare. It’s happening to your neighbor, your parent, maybe even you. And the scary part? Up to 400,000 of those cases are completely preventable. This isn’t about bad doctors or careless nurses. It’s about a system that’s still too fragile when it comes to something as basic as giving the right drug, in the right dose, to the right person. That’s what medication safety is all about - making sure medicine helps, not hurts.
What Exactly Is Medication Safety?
Medication safety isn’t just about avoiding mistakes. It’s a whole system designed to protect you from harm every step of the way - from when a doctor writes a prescription, to when you swallow the pill at home. The National Patient Safety Foundation defines it as being free from accidental injury caused by medical care during the medication-use process. That means it covers everything: how the drug is prescribed, how it’s filled at the pharmacy, how it’s given in the hospital, and how you take it at home.
Think of it like a chain. If one link breaks - say, a handwritten script is misread, or a nurse gives the wrong dose because they’re rushed - the whole chain fails. And the damage? It’s real. Adverse drug events (ADEs) include allergic reactions, overdoses, underdoses, and dangerous interactions between drugs. These aren’t just side effects you can ignore. They’re preventable injuries.
The process isn’t simple. There are nine stages where things can go wrong: procurement, storage, prescribing, transcribing, preparing, dispensing, administering, documenting, and monitoring. Each one is a chance for error. And the data shows where things break most often. Prescribing errors make up 38% of all mistakes. Administration errors - like giving a pill by mouth when it should’ve been injected - are 26%. Dispensing errors? 16%. These aren’t just numbers. They’re moments where someone’s life could change forever.
Why It Matters More Than You Think
Medication safety isn’t just for hospitals. It’s for your kitchen table. For your elderly parent who takes seven pills a day. For your child who needs liquid medicine measured in milliliters. For your friend who skipped a dose because the co-pay was too high.
Some groups are at higher risk. Children make up 20% of all medication-related emergency visits. People over 65 account for half of all hospitalizations due to adverse drug events. Pregnant women face unique risks - some medications can harm a developing baby, even if they’re safe for everyone else. And it’s not just about the drugs themselves. It’s about how they’re used.
Here’s something most people don’t realize: 42% of older adults admit to changing their meds without telling their doctor. They skip doses to save money. They double up because they forgot. They stop taking something because they felt fine. These aren’t rebellious acts - they’re desperate choices made in a system that doesn’t make it easy to stay safe.
And the cost? Not just in suffering. The U.S. healthcare system spends about $42 billion a year cleaning up preventable medication errors. That’s money that could go to better care, better equipment, better support for patients. Instead, it’s spent on ER visits, longer hospital stays, and treating complications that never should’ve happened.
The High-Risk Medications You Need to Know
Not all drugs are created equal when it comes to danger. Some are so powerful, even a tiny mistake can be deadly. These are called high-alert medications. The Institute for Safe Medication Practices (ISMP) keeps a list. The big ones:
- Insulin - involved in 17% of serious errors. Too much can send someone into a coma.
- Opioids - 14% of serious errors. Overdose can stop breathing.
- Anticoagulants (like warfarin or Eliquis) - 12% of errors. Wrong dose can cause internal bleeding.
- Intravenous oxytocin - used in labor. Too much can trigger dangerous contractions.
If you or a loved one is on any of these, extra care isn’t optional. It’s essential. That means double-checking the dose. Asking the pharmacist to explain it again. Making sure the doctor knows every other drug you’re taking. These aren’t paranoid steps - they’re survival steps.

How Technology Is Helping - and Hurting
Technology has changed the game. Electronic health records (EHRs) with built-in alerts have cut serious errors by 48%. Barcode scanners that match your wristband to your pill have reduced administration mistakes by 65%. That’s huge.
But tech isn’t perfect. Too many alerts? Doctors and nurses start ignoring them. That’s called alert fatigue. When a system gives more than 25 alerts per patient encounter, its effectiveness drops by 30%. That’s like crying wolf too many times - eventually, no one listens.
And then there’s telehealth. Since 2022, telehealth medication errors have jumped 300%. Why? No physical exam. No visual check of the patient. No way to see if they’re actually swallowing the pill. Prescribing over Zoom sounds convenient - until someone gets the wrong dose because the doctor didn’t know they were on another drug.
There’s also the problem of cost. Installing a full medication safety system in a 100-bed hospital can cost $250,000. Many smaller clinics can’t afford it. So while big hospitals get smarter, the rest of the system lags behind.
What You Can Do - Right Now
You don’t need to be a doctor to keep yourself safe. Here’s what works:
- Keep a living list of every medication you take. Include the name, dose, why you take it, and when. Update it every time something changes. The CDC says patients who do this cut reconciliation errors by 45% during hospital transitions.
- Ask questions. If you don’t know why you’re taking a drug, ask. If you’re confused about the dose, ask again. Say: “Can you spell that?” or “Is this the same as the blue pill I took last month?”
- Use pill organizers. Blister packs or weekly containers cut missed doses by 60%. They’re cheap, easy, and they work.
- Know your high-alert drugs. If you’re on insulin, warfarin, or an opioid, make sure your pharmacist and doctor know you’re aware of the risks. Ask if there’s a safer alternative.
- Don’t skip doses to save money. Talk to your doctor. Ask about generic options. Ask about patient assistance programs. There are solutions - but you have to speak up.
One patient on Reddit shared how her mother was given 10mg of Xanax instead of 1mg because the doctor’s handwriting was unclear. She ended up in the hospital for three days. That could’ve been prevented with a typed prescription. Or a quick call to the pharmacy. Or just asking, “Is this right?”

The Bigger Picture: Culture Matters Too
Here’s the truth most hospitals won’t tell you: the biggest barrier to medication safety isn’t technology. It’s culture. Too many places still punish people for making mistakes instead of fixing the system that caused them.
Only 35% of healthcare organizations have non-punitive reporting systems. That means if a nurse gives the wrong drug, they’re scared to report it - not because they’re careless, but because they fear losing their job. So the error stays hidden. The same mistake happens again. And again.
Dr. Lucian Leape from Harvard put it best: “Medication safety is no longer just about catching errors; it’s about designing systems that make errors impossible to commit.” That’s the goal. Not blame. Not shame. Better design.
And it works. Hospitals that fully embrace this approach - with trained Medication Safety Officers, clear protocols, and open reporting - reduce errors by 50% to 80%. That’s not magic. That’s smart systems.
What’s Next? The Future of Safety
The FDA just started requiring all prescription labels to use standardized numeric dosing - no more “0.5 mg” that could be misread as “5 mg.” Pilot programs saw a 32% drop in decimal errors. That’s a small change with a huge impact.
AI is starting to predict errors before they happen. Early systems look at your medical history, your other meds, your lab results, and flag risks before the prescription even leaves the computer. One pilot cut potential adverse events by 40%.
Blockchain is being tested to track where drugs come from - stopping counterfeit pills from reaching pharmacies. In Europe, it cut fake medication incidents by 65%.
And globally, the WHO’s “Medication Without Harm” campaign is pushing for a 50% reduction in preventable harm by 2027. Countries that joined saw an 18% drop in just one year.
But none of this matters if patients stay silent. If we accept that “mistakes happen” as normal. If we don’t ask questions. If we don’t speak up when something feels wrong.
Final Thought: Your Safety Is Your Right
Medication safety isn’t just a hospital policy. It’s your right. You deserve to take your medicine without fear. You deserve to know what you’re taking and why. You deserve to be heard when something doesn’t feel right.
The system isn’t perfect. But it’s getting better - because people like you are asking for more. Keep your list. Ask your questions. Trust your gut. If a pill looks different, say so. If the dose seems too high, double-check. You’re not being difficult. You’re being smart.
Because in the end, medication safety isn’t about doctors or nurses or technology. It’s about you - and the simple, powerful act of speaking up.




January 29, 2026 AT 08:12 AM
OMG I CANT BELIEVE THIS ISNT COMMON KNOWLEDGE!! My grandma took 10x her insulin dose bc the script looked like 10mg not 1mg?? She ended up in the ER for 3 days 😭 I swear if we had a pill organizer and asked one question… it could’ve been avoided. PEOPLE NEED TO KNOW THIS.
January 29, 2026 AT 16:13 PM
my doc prescribes everything electronically now but still sometimes the pharmacy messes up the dose. i just call them and say ‘hey this pill looks weird’ and they fix it. no big deal. just speak up.
January 30, 2026 AT 00:16 AM
they’re lying. 90% of these ‘errors’ are caused by people not reading the label. the system’s fine. it’s the patients who are dumb. also why do we even need pills anymore? the government should just inject us with the right stuff. #conspiracy
January 31, 2026 AT 16:23 PM
❤️ this is so important!! My mom’s on warfarin and we use a pill organizer + a little whiteboard with the schedule. It’s tiny effort for huge peace of mind. 🙌 also, always ask ‘is this generic?’ - saved us $80/month 😊
February 1, 2026 AT 19:24 PM
While the statistical data presented is compelling and aligns with peer-reviewed literature on adverse drug events, it is worth noting that systemic reform requires not only individual vigilance but also institutional accountability. The cultural resistance to non-punitive error reporting remains a significant barrier to scalable improvement in medication safety protocols across primary care settings.
February 2, 2026 AT 14:00 PM
i cried reading this. my aunt died from a drug interaction because her cardiologist didn’t know she was taking that herbal supplement. nobody asked. nobody checked. it’s not her fault. it’s the system’s. and now i make sure EVERYONE i know has a meds list. even my dog’s vet gets it. 🥺
February 3, 2026 AT 10:19 AM
the epistemological framework underlying medication safety discourse is predicated on a positivist assumption of linear causality - yet human agency and pharmacological complexity defy reductionist models. alert fatigue is not a design flaw, it’s a symptom of ontological dissonance in technocratic healthcare.
February 5, 2026 AT 04:09 AM
Oh wow, so we’re supposed to be our own pharmacists now? Because clearly, the $200k hospital systems are too lazy to get it right. Let me just take my 7 pills, read the tiny font, and guess if this blue one is the one that doesn’t kill me. Thanks for the sarcasm, I needed that.
February 7, 2026 AT 00:37 AM
Keep a list. Ask questions. Use organizers. These are low-cost, high-impact actions. The data supports it. Simple. Done.
February 7, 2026 AT 06:24 AM
In India, we have no such problems. Our doctors are trained in ancient Ayurvedic precision. These American statistics are propaganda to sell EHRs. Also, your insulin is probably laced with microchips. Why do you think they want you dependent?
February 7, 2026 AT 22:19 PM
Stop being passive. If your doctor won’t type a prescription, find a new one. If your pharmacy gives you the wrong pill, report them. If you don’t know what you’re taking, you’re not a patient-you’re a lab rat. And stop blaming the system. Fix it yourself. Now.
February 9, 2026 AT 07:41 AM
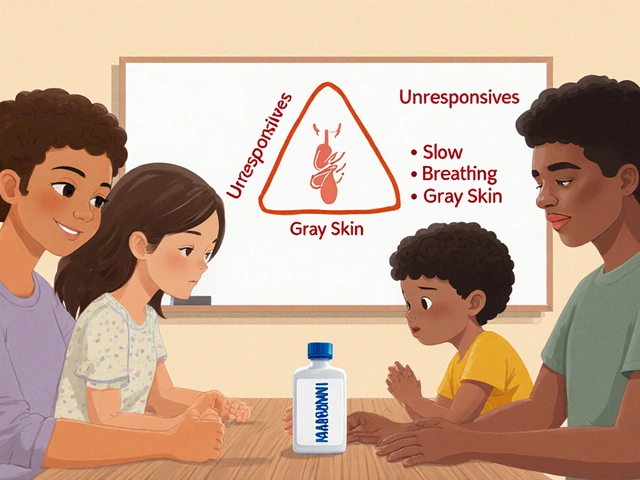
THIS. My cousin was on opioids after surgery and didn’t know the risks. We sat down with her and her mom and made a little chart with pics of the pills and dosing times. She’s doing amazing now 😊 never underestimate the power of a printed list + a hug 💪❤️
February 10, 2026 AT 10:53 AM
While the Western model of pharmacovigilance is commendable, one must acknowledge the structural inequities in global access. In rural India, a patient may wait three weeks for a refill. Safety is a luxury. Perhaps we should first ensure access before demanding compliance with complex protocols. 🤔