Blood Thinner & Turmeric Risk Checker
Risk Assessment Tool
Enter your details below to assess the risk of dangerous interactions between turmeric supplements and your blood thinner medication.
Your Risk Assessment
Based on your inputs, there is a high risk of dangerous interactions between your blood thinner and turmeric supplements. The combination of blood thinners and turmeric (especially with black pepper) can significantly increase bleeding risk and may lead to hospitalization.
Why this is dangerous: Turmeric contains curcumin which interferes with blood clotting. Black pepper increases curcumin absorption by up to 2,000%, and it also blocks liver enzymes that normally break down blood thinners. This creates a dangerous accumulation of both substances in your body.
Recommended Action
Stop taking turmeric supplements immediately. Consult your doctor before taking any further supplements while on blood thinners. Never assume "natural" means safe.
What to Watch For
Watch for unusual bruising, nosebleeds, blood in stool or urine, dark urine, yellow skin or eyes, nausea, or extreme fatigue. These could be signs of bleeding or liver damage.
Every year, millions of Americans take turmeric supplements hoping for less inflammation, better joint health, or a natural boost to their immune system. Many of these supplements also include black pepper - marketed as a way to make turmeric work better. But if you're on a blood thinner like warfarin, apixaban, or clopidogrel, this combo could be dangerous. It’s not a myth. It’s not a rumor. It’s documented in medical journals, hospital case reports, and government health alerts.
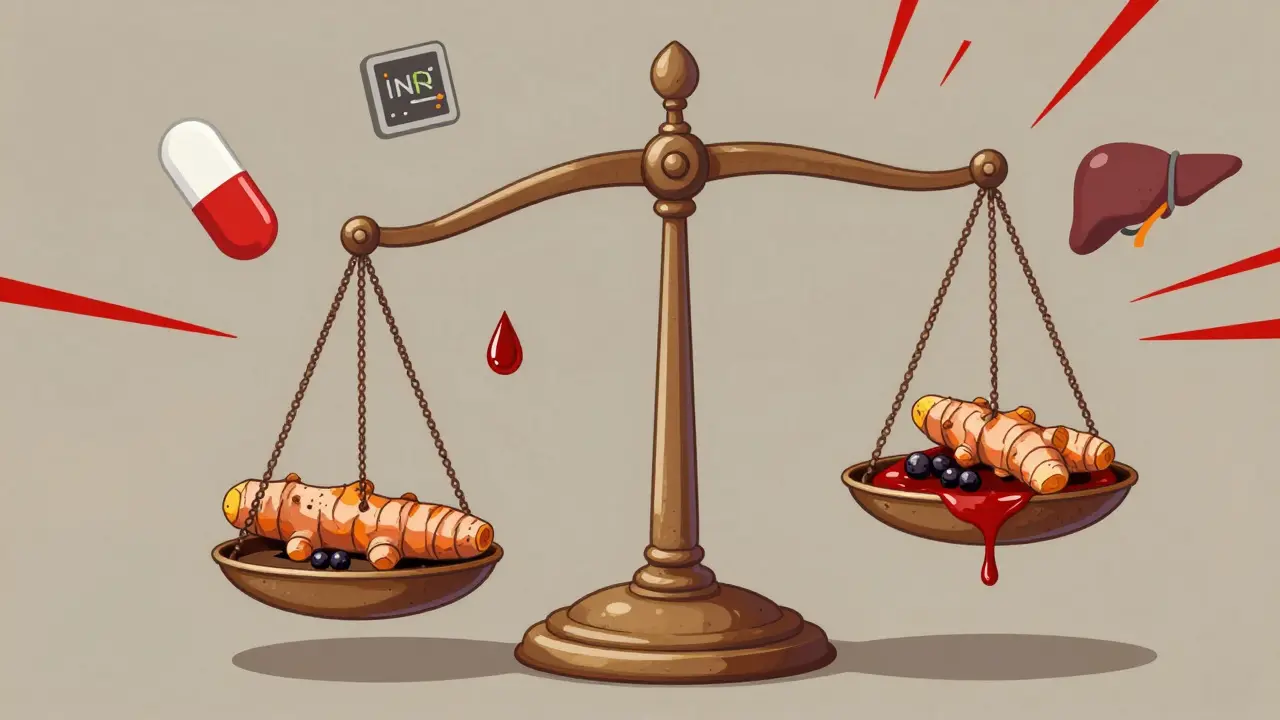
Why Turmeric and Blood Thinners Don’t Mix
Turmeric contains curcumin, a compound that naturally interferes with blood clotting. It does this by reducing platelet aggregation - meaning your blood cells have a harder time sticking together to form clots. That sounds good if you’re trying to prevent heart attacks or strokes. But if you’re already on a prescription blood thinner, adding turmeric pushes your body past the safety line.Think of your blood as a balancing act. Blood thinners keep it from clotting too much. Too little clotting, and even a small cut can turn into serious bleeding. Too much, and you risk a clot. Turmeric tips that balance. A 2024 report from the Welsh Medicines Advice Service tracked a patient on stable warfarin therapy whose INR (a key blood clotting measurement) jumped from 2.5 to 6.8 - a level that puts you at high risk for internal bleeding - after starting a daily turmeric supplement. That’s not rare. It’s been seen in multiple clinical cases.
Black Pepper Makes It Worse - A Lot Worse
Here’s where things get riskier. Most turmeric supplements include black pepper extract, or piperine, because it boosts curcumin absorption by up to 2,000%. That sounds like a win - until you realize your liver can’t handle it.Piperine doesn’t just help curcumin get into your bloodstream. It also blocks liver enzymes (CYP3A4 and P-glycoprotein) that normally break down both curcumin and many blood thinners. That means your body doesn’t clear the drugs the way it should. The result? Higher levels of both the supplement and the medication floating around at the same time.
That’s not theoretical. A 2023 MDVIP analysis showed that combining turmeric and black pepper can create a 20-fold increase in curcumin concentration compared to turmeric alone. For someone on warfarin, that’s like doubling or tripling their dose without knowing it. And warfarin is especially tricky - it has a narrow therapeutic window. The difference between a safe dose and a toxic one is tiny. Even a small change can land you in the ER.
Which Blood Thinners Are Most at Risk?
Not all blood thinners react the same way, but turmeric and black pepper can interfere with nearly all of them:- Warfarin (Coumadin): Highest risk. INR levels spike unpredictably. The Welsh Medicines Advice Service calls this the most dangerous combination.
- Apixaban (Eliquis), Rivaroxaban (Xarelto), Dabigatran (Pradaxa): Direct oral anticoagulants (DOACs). Less studied than warfarin, but animal studies show curcumin increases their blood levels significantly.
- Clopidogrel (Plavix): A platelet inhibitor. Turmeric adds to its effect, increasing bruising and bleeding risk.
- Aspirin, Ibuprofen, Naproxen: These are NSAIDs - they already thin blood. Turmeric stacks on top of that.
- Heparin, Enoxaparin (Lovenox), Dalteparin (Fragmin): Injectable anticoagulants. Turmeric doesn’t directly interact with them, but it still increases overall bleeding risk.
The American Heart Association estimates 8.4 million Americans take anticoagulants. About 2.2 million of them are on warfarin. And according to Nutrition Business Journal, over 18% of U.S. adults took turmeric supplements in 2022. That’s millions of people unknowingly mixing a high-risk combo.
Dietary Turmeric Is Different - But Supplements Aren’t
There’s a big difference between eating turmeric in your curry and popping a 500 mg capsule.One teaspoon of ground turmeric in food contains about 200 mg of curcumin - and your body absorbs less than 1% of it naturally. That’s not enough to interfere with blood thinners. Multiple studies, including one from Healthline in 2022, confirm that culinary use doesn’t raise bleeding risk.
But supplements? A single capsule can contain 500-1,000 mg of curcumin - and with black pepper, absorption jumps to 20%. That’s the equivalent of eating 10-20 teaspoons of turmeric powder in one go. And that’s exactly what the liver and blood system are forced to handle.
Real Stories: What Happens When People Ignore the Warnings
Medical forums are full of stories that should make anyone think twice.One user on HealthUnlocked reported hospitalization after three weeks of taking “one teaspoon of turmeric supplement daily” while on apixaban. He developed gastrointestinal bleeding - a serious, life-threatening condition.
Another person on Reddit’s r/bloodthinners shared that they started bruising easily after adding turmeric-black pepper capsules. Their doctor found their INR was dangerously high. They stopped the supplement, and the bruising faded in two weeks.
Then there’s the liver damage. MDVIP’s 2023 report details cases where patients developed jaundice, dark urine, nausea, and extreme fatigue within weeks of starting turmeric-black pepper supplements. These are signs of liver injury - and piperine is partly to blame. It stresses the liver by blocking detox pathways.
And it’s not just about interactions. ConsumerLab’s 2022 testing found that 30% of turmeric supplements contained lead levels above California’s safety limits. So you’re not just risking bleeding - you might be poisoning yourself.
What Doctors Are Saying Now
The medical community is unified: avoid turmeric supplements if you’re on blood thinners.The Cleveland Clinic’s Dr. Bishop says bluntly: “Don’t take turmeric supplements if you’re on warfarin or any other anticoagulant.” He points out that patients often don’t tell their doctors about supplements. A 2022 JAMA study found 42% of patients hide their supplement use.
The British Heart Foundation says: “Check with your GP first.” Simple. Direct. But most people don’t.
The American College of Cardiology updated its guidelines in March 2024 to say: “Complete avoidance of turmeric supplements is recommended for patients on warfarin. Use with caution - if at all - with DOACs.”
And here’s the kicker: only 41% of turmeric supplement labels include warnings about blood thinner interactions - even though the FDA requires it under the Dietary Supplement Health and Education Act of 1994. You’re not being warned. You’re being left in the dark.
What Should You Do?
If you’re on a blood thinner:- Stop taking turmeric supplements immediately. This includes anything labeled “turmeric with black pepper,” “bioavailable curcumin,” or “enhanced absorption.”
- Don’t assume “natural” means safe. Natural doesn’t mean non-toxic. Many of the deadliest drug interactions come from herbs and supplements.
- Keep eating turmeric in food. One to two teaspoons a day in cooking is fine. The dose is too low to matter.
- Tell your doctor about every supplement you take. Even if you think it’s harmless. Write it down. Bring the bottle.
- Watch for signs of bleeding or liver damage. Unusual bruising, nosebleeds, blood in stool or urine, dark urine, yellow skin or eyes, nausea, fatigue - get checked right away.
If you’re considering turmeric for arthritis or inflammation, talk to your doctor about safer alternatives. Omega-3s from fish oil (in controlled doses), ginger, or prescription anti-inflammatories may be better options - and they won’t risk your life.
The Bigger Picture: Why This Keeps Happening
The turmeric supplement market hit $1.14 billion in 2022. Over 60% of those products include black pepper because it sells better. Marketers don’t care about your INR. They care about your click. They care about your cart.Regulators are slow. The FDA doesn’t approve supplements before they hit shelves. They only act after harm is done. That’s why so many products lack warnings - and why people keep getting hurt.
The good news? Research is moving. A 2023 study in the Journal of Dietary Supplements is testing a new delivery system using lecithin instead of piperine. It might deliver curcumin safely without the dangerous absorption spike. But that’s still in testing. It’s not on shelves yet.
Until then, the safest choice is simple: if you’re on blood thinners, skip the capsules. Enjoy your turmeric in food. Your body will thank you.




January 18, 2026 AT 10:06 AM
Wow. I knew turmeric was popular, but I had no idea how dangerous it could be with blood thinners. This post literally saved me - I was taking a daily capsule for my knees. Stopped it today. Thanks for the clarity.
Also, eating it in curry? Still doing that. No regrets.
People need to stop assuming ‘natural’ = safe. That’s how we get here.
January 18, 2026 AT 15:03 PM
so like… black pepper makes it worse??? no way
wait no wait
oh wait
oh no
im on eliquis
im dead
January 19, 2026 AT 04:00 AM
THIS. This is the kind of info we need more of. Not just scare tactics - real, documented, clinical facts. I work in pharmacy and I see this ALL the time. Patients come in saying ‘my doctor didn’t ask’ and I’m like… you didn’t tell them either.
Bring the bottle. Write it down. Say it out loud. Your life depends on it.
Also - yes, turmeric in food is fine. But supplements? No. Not worth it. Your body doesn’t need it that badly.
January 20, 2026 AT 19:04 PM
One must contemplate the deeper metaphysical implications of this phenomenon: the commodification of ancient wisdom into profit-driven capsules, stripped of context, ritual, and ancestral understanding. The Ayurvedic tradition never prescribed isolated curcumin with piperine as a pharmacological intervention - it was always part of a holistic regimen, with diet, breath, and intention.
Today, the pharmaceutical-industrial complex has weaponized the very essence of healing, packaging it with deceptive labels and predatory marketing. The FDA’s inaction is not negligence - it is complicity.
Are we truly free when our bodies are manipulated by unregulated substances sold as ‘wellness’? The answer lies not in the supplement bottle, but in the soul of our collective surrender to convenience.
January 21, 2026 AT 03:09 AM
Let me be brutally clear: anyone who takes turmeric supplements while on anticoagulants is not just ignorant - they’re reckless. Curcumin is a potent COX-2 and thromboxane inhibitor. Piperine is a CYP3A4/P-gp inhibitor. These are not vague herbal ‘effects.’ These are biochemical mechanisms with documented pharmacokinetic consequences.
The Welsh case report you cited? That’s not an outlier. It’s a textbook example of a Class I drug-herb interaction. The INR spike to 6.8? That’s not ‘a bit high.’ That’s a hemorrhagic catastrophe waiting to happen.
And yet - people still buy it. Why? Because they’d rather trust a YouTube influencer with 300k followers than their own hematologist. The tragedy isn’t the supplement - it’s the epistemic collapse of public health literacy.
January 21, 2026 AT 11:16 AM
Oh honey. You think this is bad? Try explaining to a Canadian doctor why your ‘natural’ supplement from India has lead levels higher than a 1970s toy. We’ve got kids in Toronto with elevated blood lead from ‘immune boosters’ imported from Delhi.
And don’t get me started on the ‘bioavailable’ nonsense. That’s just corporate jargon for ‘we made it poison faster.’
Canada’s got stricter rules. We don’t let this crap fly under the radar. You folks in the US are playing Russian roulette with your liver.
January 22, 2026 AT 18:58 PM
Hi, I just wanted to say… I’m so glad you wrote this. I’ve been feeling so guilty because I took turmeric for a year while on warfarin… I didn’t know! I thought it was ‘just a spice’…
My INR was 4.2 last month - my doctor said I was ‘lucky’ it didn’t go higher. I’ve stopped everything. I feel so stupid. But I’m learning. And I’m telling everyone now.
You’re not judging me, right? I just… I didn’t know.
Thank you for being so clear. I’m going to bring my supplement bottle to my next appointment. I promise.
January 23, 2026 AT 01:37 AM
lol i just took turmeric with black pepper yesterday for my knee pain and now im scared
but like… its just one capsule right??
maybe i should just stop
or maybe i should keep going and hope for the best
idk
January 23, 2026 AT 12:23 PM
As someone who grew up in Kerala, we use turmeric in everything - rice, dals, even milk. But we never took it in pills. It was always food. Always in small amounts. Always with context.
This isn’t about ‘natural vs synthetic.’ It’s about respect. Respect for the medicine, respect for the body, respect for the science.
And honestly? The real danger isn’t the supplement - it’s the silence. People don’t talk about this because they’re embarrassed. But we need to talk. Loudly.
Thanks for breaking the silence.
January 24, 2026 AT 19:31 PM
I just wanted to add - if you’re on warfarin, please, please, please get your INR checked regularly, even if you think you’re fine. And if you’ve taken turmeric in the last 2 weeks, tell your lab. They need to know.
Also - if you’re taking any other supplements (garlic, ginger, ginkgo, fish oil, vitamin E) - same rule applies. They all interact.
And yes, I know it’s annoying to list everything… but your life is worth the extra 2 minutes.
January 26, 2026 AT 15:53 PM
While the post presents a compelling argument grounded in pharmacological literature, it is imperative to acknowledge the absence of randomized controlled trials (RCTs) quantifying the precise magnitude of interaction between piperine-enhanced curcumin and direct oral anticoagulants (DOACs).
Although case reports and in vitro studies suggest a plausible mechanism, extrapolating these findings to clinical populations requires caution. The pharmacokinetic variability among individuals, compounded by dietary factors and genetic polymorphisms in CYP3A4 and P-glycoprotein, renders generalized recommendations potentially overbroad.
Until robust RCTs are conducted, the recommendation for complete avoidance - while prudent - may not be universally evidence-based. A tiered risk assessment, rather than blanket prohibition, may be more scientifically rigorous.