The link between trigeminal neuralgia and cluster headaches is more than a coincidence. Both conditions unleash excruciating facial pain, yet they arise from different triggers and pathways. Understanding how they intersect helps patients get the right diagnosis and a treatment plan that tackles both.
When a sudden, electric‑shock‑like pain hits one side of the face, doctors often think of Trigeminal Neuralgia - a chronic nerve‑pain disorder affecting the trigeminal nerve (cranial nerve V) that causes brief, intense facial pain. The pain usually lasts seconds to minutes but can repeat dozens of times a day.
On the other side of the spectrum, Cluster Headaches - a primary headache disorder marked by severe, unilateral orbital pain accompanied by autonomic symptoms strike in episodes or "clusters" that can last weeks or months, followed by remission periods.
What Is Trigeminal Neuralgia?
Trigeminal Neuralgia (TN) is most often caused by Vascular Compression - the pressure of a blood vessel, typically the superior cerebellar artery, on the trigeminal root. The compression irritates the nerve sheath, leading to ectopic firing of pain signals. Classic TN follows a “trigger zone” where light touch, chewing, or even a breeze can provoke an attack.
Key characteristics:
- Sharp, stabbing pain lasting < 2 minutes
- Occurs in episodes of 10‑100 attacks per day
- Most common in people aged 50‑70
First‑line pharmacotherapy is Carbamazepine - an anticonvulsant that stabilizes hyperactive neuronal membranes. When meds fail, microvascular decompression surgery offers lasting relief for many.
What Are Cluster Headaches?
Cluster Headaches (CH) belong to the trigeminal autonomic cephalalgias (TACs). The pain is typically deep, boring, and orbital, lasting 15‑180 minutes per attack. Unlike TN, CH is accompanied by autonomic signs such as tearing, nasal congestion, eyelid drooping, and facial sweating.
Typical patterns:
- One or two attacks per hour during a cluster period
- Clusters occur seasonally (often in spring or autumn)
- Male predominance; onset often in the 20s‑40s
Treatment relies on fast‑acting therapies: high‑flow Oxygen Therapy - inhaling 100% oxygen at 12‑15 L/min for 15 minutes aborts most attacks, while preventive meds like Verapamil - a calcium‑channel blocker used daily to reduce attack frequency are used between clusters.
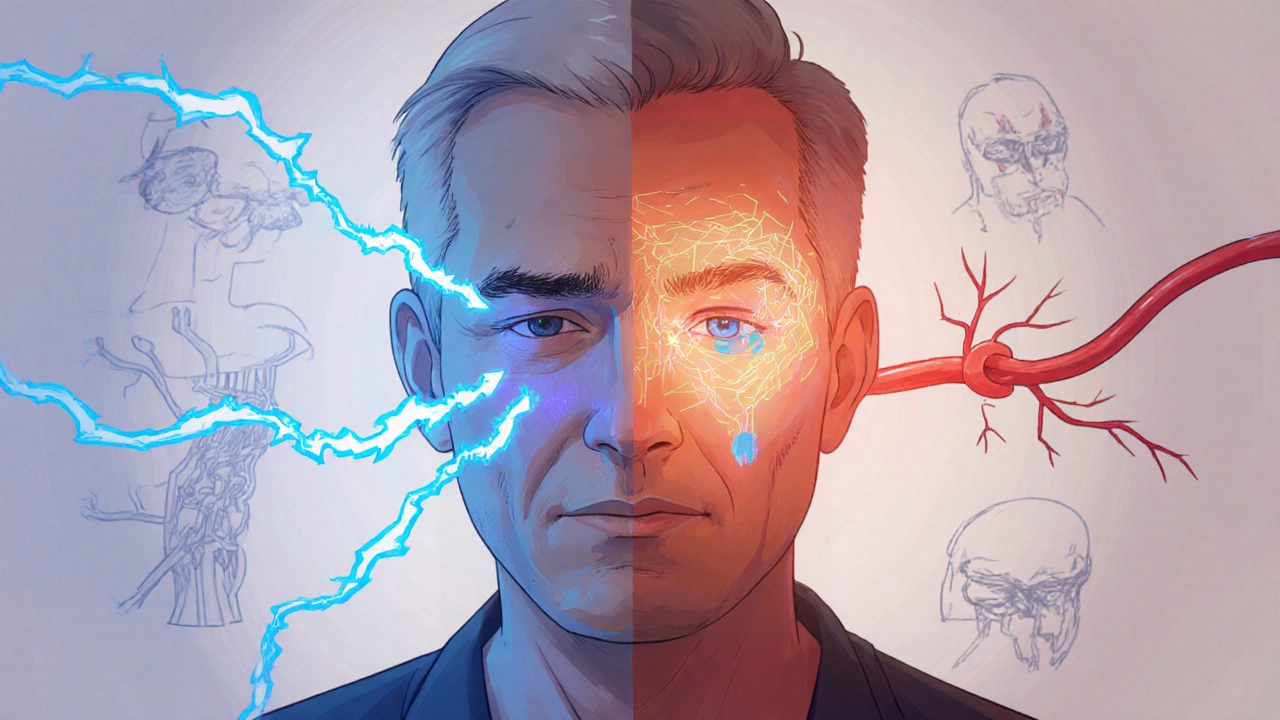
Shared Neurovascular Mechanisms
Both TN and CH involve the trigeminal system, but their pathways intersect at several points:
- Vascular contact: In TN, the superior cerebellar artery directly compresses the nerve. In CH, imaging often reveals Calcitonin Gene‑Related Peptide - a neuropeptide that mediates vasodilation and pain transmission release from trigeminal afferents, causing the characteristic vascular changes.
- Hypothalamic involvement: Functional MRI studies show hypothalamic activation during CH attacks, and emerging data suggest hypothalamic dysregulation may also sensitize the trigeminal nucleus, worsening TN pain.
- Autonomic overlap: While TN is classically painless between attacks, some patients report tearing or nasal congestion, hinting at a shared Autonomic Nervous System - the part of the peripheral nervous system controlling involuntary functions component.

Clinical Overlap and Diagnostic Challenges
Because both disorders produce unilateral facial pain, misdiagnosis is common. Here are red flags that help separate them:
- Duration: TN attacks are seconds; CH attacks last minutes to hours.
- Accompanying signs: CH comes with autonomic symptoms (lacrimation, nasal stuffiness); TN usually does not.
- Trigger patterns: TN often has a specific trigger zone; CH attacks can occur spontaneously, often at night.
When a patient reports both short electric shocks and longer, tearing attacks, clinicians should consider co‑occurrence. High‑resolution Magnetic Resonance Imaging - a non‑invasive scan that visualizes nerve‑vessel relationships can reveal vascular compression while also ruling out secondary causes.
Treatment Strategies When Both Conditions Co‑exist
Managing dual diagnoses demands a layered approach:
- Address the dominant pain: If the patient’s most disabling attacks are TN‑type, start with carbamazepine or oxcarbazepine. If CH dominates, begin verapamil and prescribe acute oxygen therapy.
- Combine preventive meds cautiously: Overlap of carbamazepine and verapamil is generally safe, but monitor cardiac conduction due to verapamil’s effect on the QT interval.
- Consider procedural options: Microvascular decompression can relieve TN while having little impact on CH. For refractory CH, occipital nerve stimulation or sphenopalatine ganglion blocks may be added.
- Lifestyle tweaks: Regular sleep, avoidance of alcohol during cluster periods, and stress‑reduction techniques help both disorders.
Quick Checklist for Patients
- Document pain timing, triggers, and associated symptoms in a diary.
- Ask your neurologist about high‑resolution MRI to assess vascular compression.
- If attacks are longer than 2 minutes with tearing, discuss oxygen therapy or triptans.
- Review medication side‑effects; carbamazepine may cause drowsiness, verapamil can cause constipation.
- Consider referral to a headache specialist if you’ve tried first‑line drugs without relief.
Comparison of Trigeminal Neuralgia and Cluster Headaches
| Feature | Trigeminal Neuralgia | Cluster Headache |
|---|---|---|
| Pain quality | Sharp, electric‑shock | Dull, burning, orbital |
| Duration per attack | Seconds to 2 minutes | 15-180 minutes |
| Typical frequency | 10-100+ per day | 1-8 per hour during clusters |
| Autonomic signs | Rare | Lacrimation, nasal congestion, ptosis |
| Common age of onset | 50-70 years | 20-40 years |
| First‑line medication | Carbamazepine | Verapamil (preventive); 100% O₂ (acute) |
| Surgical option | Microvascular decompression | Occipital nerve stimulation |
Frequently Asked Questions
Can a person have both trigeminal neuralgia and cluster headaches?
Yes. Although rare, some patients experience both disorders. Overlapping trigeminal pathways and shared vascular mechanisms can cause symptoms of each to appear in the same individual.
How does MRI help differentiate the two conditions?
MRI with high‑resolution sequences visualizes the relationship between the trigeminal nerve and nearby arteries. Vascular compression points to trigeminal neuralgia, while the absence of such compression alongside hypothalamic activation hints toward cluster headaches.
Is oxygen therapy useful for trigeminal neuralgia?
Oxygen therapy is specific to cluster headaches and does not affect TN pain. However, some clinicians use it experimentally for severe facial pain, but evidence is limited.
What lifestyle changes can reduce attack frequency?
Maintain consistent sleep patterns, limit caffeine and alcohol (especially during cluster periods), manage stress through meditation or gentle exercise, and avoid known TN triggers like cold wind or chewing gum.
When should surgery be considered?
If medication fails to control pain or causes intolerable side effects, microvascular decompression is an option for TN, while occipital nerve stimulation or sphenopalatine ganglion block may be offered for refractory cluster headaches.




October 23, 2025 AT 17:51 PM
It looks like you’re trying to lump trigeminal neuralgia and cluster headaches together, but they’re not the same thing. TN is a nerve‑root problem, while CH is a hypothalamic driven headache. The treatments you need are totally different, so mixing them up can lead to a mess. Keep the two separate when you talk about meds.
November 2, 2025 AT 21:18 PM
Although the article mentions overlapping vascular mechanisms, the claim that hypothalamic dysregulation sensitises the trigeminal nucleus in TN remains largely hypothetical. Robust functional MRI data supporting this link are scarce, and most studies focus on CH alone. Moreover, carbamazepine’s efficacy does not hinge on hypothalamic activity, which further separates the pathophysiologies. Therefore, one should treat the evidence with caution before asserting a shared central driver.
November 13, 2025 AT 01:45 AM
Meh, could’ve been shorter.
November 23, 2025 AT 06:11 AM
India has produced some of the best neurologists in the world!! Their work on trigeminal pathways is world‑class and deserves more respect!! We should shout about it, not hide it!!
December 3, 2025 AT 10:38 AM
I hear your excitement and it’s great to see pride in our medical community. At the same time, balancing enthusiasm with precise language helps everyone understand the nuances. Both conditions deserve clear explanations, especially for patients navigating treatment options.
December 13, 2025 AT 15:05 PM
Pain, whether a sharp shock from TN or a burning cluster, can act as an unwanted teacher. It reminds us that the nervous system is both fragile and resilient, constantly adapting to insult. When we observe how one brain region can modulate another, we glimpse the larger tapestry of human experience. This perspective encourages humility in our clinical choices.
December 23, 2025 AT 19:31 PM
I've been dealing with both TN and CH for a few years now, and let me tell you, the overlap is more than just a textbook note. First, the electric‑sharp jabs of TN can start in the morning while I'm still half asleep, and then a few weeks later a cluster episode will hit me at night, waking me up with tears and a pounding ache. I keep a detailed diary, noting the exact time, weather, and what I ate, because patterns can be sneaky. One thing I discovered is that stress seems to amplify both types, even though the triggers look different on paper. When I'm under a lot of pressure at work, I notice the TN attacks become more frequent, and the cluster periods seem to last longer. High‑resolution MRI was a game changer for me; it showed a tiny artery pressing on my trigeminal root, confirming the TN diagnosis, while also ruling out other issues that could mimic CH. My neurologist started me on carbamazepine, which dulled the TN shocks but left the cluster attacks untouched. For the clusters, we introduced high‑flow oxygen therapy, and I was amazed at how quickly it could abort an episode, sometimes within minutes. Verapamil was added later as a preventive, and after a few months the frequency dropped dramatically. I also experimented with lifestyle tweaks: regular sleep, cutting back on caffeine, and avoiding alcohol during cluster seasons. Meditation helped reduce the overall stress load, and I found that gentle jaw exercises didn't trigger TN as much as chewing gum used to. Surgery was considered for the TN but I decided to hold off because the meds were working well enough, and I wasn’t comfortable with the risks yet. The biggest lesson I've learned is that you have to treat each condition on its own terms, even if they share some neurovascular pathways. Having both diagnoses can feel overwhelming, but with a structured plan and a good support team, you can regain a decent quality of life. Remember, documenting every detail is crucial – it gives your doctor the data they need to fine‑tune treatment. Stay hopeful and keep pushing for answers, because the science is constantly evolving.
January 2, 2026 AT 23:58 PM
Thank you for sharing such a thorough personal journey; it really grounds the discussion in real‑world experience. Your point about stress influencing both disorders highlights the need for holistic management. Encouraging patients to keep a pain diary is an excellent practical tip that many clinicians overlook. Keep championing that balanced approach of medication, lifestyle, and careful monitoring.
January 13, 2026 AT 04:25 AM
Great info, thx!
January 23, 2026 AT 08:51 AM
Glad you found it helpful! A quick thank‑you goes a long way in these communities.
February 2, 2026 AT 13:18 PM
When discussing overlapping pain syndromes, it's vital to differentiate the duration and autonomic signs; this helps avoid misdiagnosis!!! Also, remember that patient education on trigger avoidance can dramatically reduce the burden!!!
February 12, 2026 AT 16:51 PM
While the enthusiasm is noted, the discourse would benefit from a more scholarly tone. Let’s elevate the conversation beyond emojis and emotive exclamations 🌟📚.