Maintaining an active lifestyle despite an enlarged prostate is crucial for overall health and well-being. First, it's important to consult with a healthcare professional for any necessary treatments or recommendations. Incorporating regular exercise, such as walking or swimming, can help alleviate symptoms and maintain physical fitness. Additionally, paying attention to a balanced diet and staying well-hydrated can support prostate health. Lastly, practicing stress management techniques, such as meditation or yoga, can positively impact an individual's mental and emotional health during this time.
Enlarged Prostate (BPH): What You Need to Know
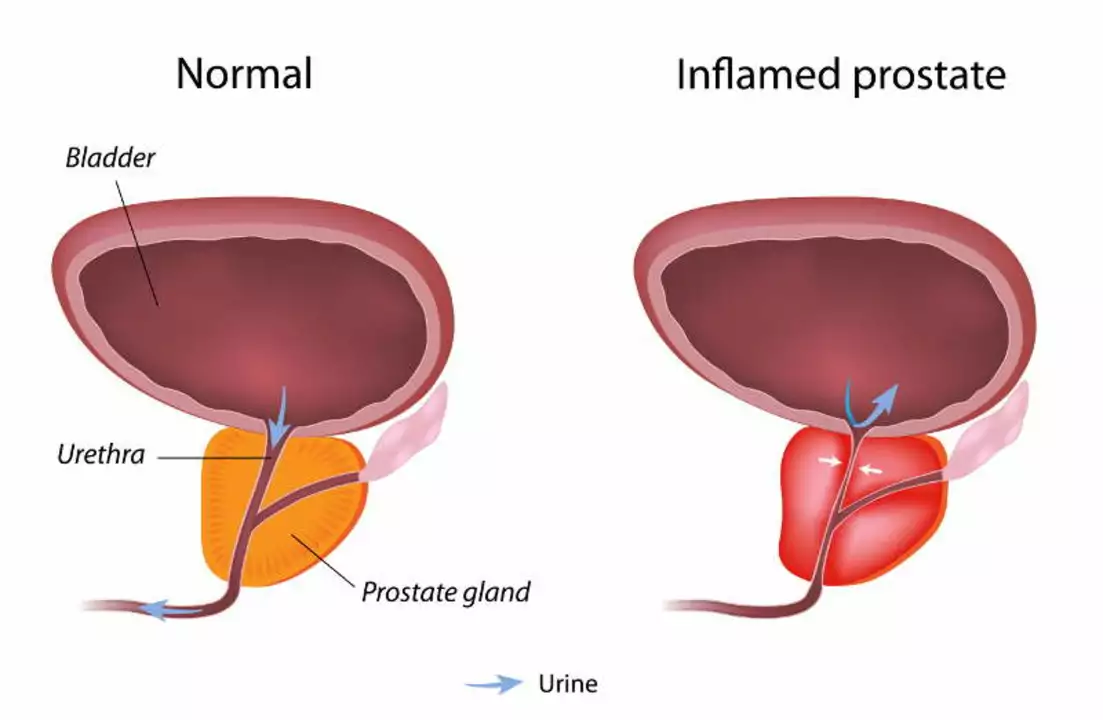
If you’ve heard friends or family mention an "enlarged prostate," they’re talking about a condition called benign prostatic hyperplasia, or BPH. It’s not cancer, but the gland gets bigger and can mess with how you pee. Most men notice changes after age 50, though it can start earlier.
Why does it happen? The prostate is made of muscle and gland tissue that grow a little each year. Hormones like testosterone turn into dihydrotestosterone (DHT) in the prostate, and DHT nudges cells to multiply. Over time, that extra tissue squeezes the urethra – the tube that carries urine out of your body.
Typical Symptoms and When to See a Doctor
The biggest clue is how often you have to go. You might feel a sudden urge, need to get up at night (called nocturia), or notice a weak stream. Some men can’t finish emptying their bladder, which feels uncomfortable.
These signs are common, but they’re worth a check‑up if they start affecting your sleep, work, or social life. A quick office visit can include a digital rectal exam and maybe an ultrasound to see how big the gland is.
Don’t ignore pain or blood in urine – those could signal infection or stones instead of plain BPH. If you get any of those, call your doctor right away.
Common Treatment Paths
Most men manage BPH without surgery. Lifestyle tweaks help a lot: limit caffeine and alcohol, avoid drinking fluids before bedtime, and practice “double voiding” – pee, wait a minute, then try again to empty the bladder fully.
If symptoms stay stubborn, doctors often prescribe medication. Alpha‑blockers (like tamsulosin) relax prostate muscles so urine flows easier. Another class, 5‑alpha‑reducing drugs (such as finasteride), shrink the gland over months by lowering DHT levels.
Some men combine both types for faster relief. Side effects are usually mild – dizziness or reduced libido – but your doctor will weigh benefits against risks.
When medicine isn’t enough, minimally invasive procedures step in. A common option is transurethral microwave therapy (TUMT) that uses heat to shrink tissue. Another is the water‑jet technique called UroLift, which lifts and holds open the prostate without cutting it.In rare cases where the gland is very large or complications arise, surgery like transurethral resection of the prostate (TURP) may be recommended. Recovery takes a few weeks, and most men regain normal urination.
Remember, BPH isn’t a one‑size‑fits‑all problem. Your doctor will look at prostate size, symptom severity, and overall health before suggesting a plan.
While you’re exploring options, keep a simple log of bathroom trips – time, frequency, any pain. That record helps your clinician see patterns and adjust treatment quickly.
Finally, stay informed but avoid panic‑selling supplements that claim to shrink the prostate overnight. Some herbs like saw palmetto have mixed results, and they can interact with prescription meds.
The good news is most men find relief through a mix of lifestyle changes, medication, or minor procedures. Talk openly with your doctor, track your symptoms, and you’ll likely get back to a normal routine without constant bathroom trips.