Nasal Decongestant Risk Calculator
How Long Have You Used Nasal Decongestant Sprays?
Have you ever used a nasal decongestant spray for a cold, only to find that your nose gets more blocked the longer you use it? You’re not alone. What feels like a worsening cold might actually be something called rhinitis medicamentosa - a condition caused by overusing nasal decongestant sprays. It’s not a cold. It’s not allergies. It’s your own nose reacting to the medicine you thought was helping.
How a Quick Fix Turns Into a Long-Term Problem
Nasal decongestant sprays like Afrin, Neo-Synephrine, or Otrivin work fast. They shrink swollen blood vessels in your nose, giving you instant relief. But that relief is temporary. After a few hours, the effect wears off. And if you keep spraying, your body starts to depend on it. Instead of staying open, your nasal passages get even more swollen than before - a phenomenon called rebound congestion. This isn’t just a myth. Studies show that using these sprays for more than three to four days straight increases your risk of rebound congestion by up to 92%. The nasal lining becomes inflamed, red, and swollen. Over time, it can even turn dry, crusty, and irritated. The more you spray, the worse it gets - until you’re stuck in a cycle where you feel like you can’t breathe without the spray. The active ingredients behind this problem are usually oxymetazoline, phenylephrine, or xylometazoline. These are common in over-the-counter sprays sold in pharmacies across Australia, the U.S., and Europe. The FDA now requires these products to have clear warning labels saying “Do not use more than 3 days.” But many people still miss it. They think, “I’m just using it as needed,” not realizing that “as needed” becomes “every 4 hours” - and then “I can’t go a day without it.”What Rhinitis Medicamentosa Really Feels Like
If you’ve been using nasal sprays for more than a week, you might already be dealing with rhinitis medicamentosa. Symptoms include:- Constant nasal blockage, even without a cold or allergies
- Worsening congestion after the spray wears off
- Need to spray more frequently just to feel normal
- Dry mouth or throat from breathing through your mouth
- Snoring or trouble sleeping because you can’t breathe through your nose
- Red, swollen, or irritated nasal lining when checked by a doctor
The Only Way to Break the Cycle: Stop the Spray
The hard truth? The only way to fix rebound congestion is to stop using the decongestant spray completely. There’s no magic pill. No shortcut. No way around it. But stopping cold turkey can be brutal. For the first 3-7 days, your congestion will likely get worse. That’s normal. Your blood vessels, used to being constricted, now overreact and swell even more. Many people give up during this phase and go right back to the spray - which resets the whole cycle. That’s why the most successful approach isn’t just stopping - it’s stopping strategically. The Mayo Clinic recommends a simple trick: stop using the spray in one nostril first. Wait until that side clears up - which can take 3-5 days - then stop in the other nostril. This reduces the shock to your system. You’re still breathing through one side while the other heals. Many patients report this method makes withdrawal much more manageable.
What to Use Instead: Proven Alternatives
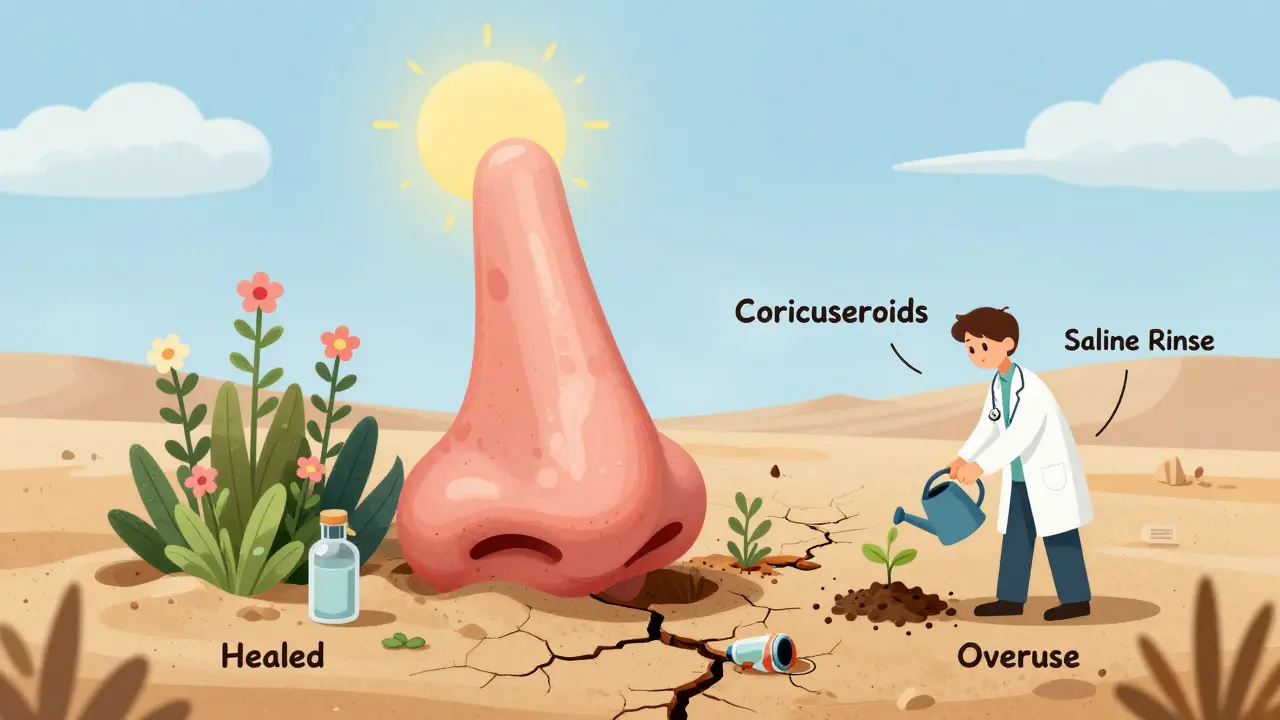
While you’re weaning off the spray, you need something to help with the symptoms. Here’s what actually works, backed by clinical studies:1. Intranasal Corticosteroids
These are the gold standard. Sprays like Flonase (fluticasone) or Nasonex (mometasone) reduce inflammation in your nasal lining - the exact problem causing the congestion. Unlike decongestants, they don’t cause rebound. They take a few days to work, but they fix the root cause. Studies show 68-75% of people see major improvement after using corticosteroids daily for 2-4 weeks during withdrawal. Use them twice a day at first, then cut to once daily as symptoms improve. Don’t stop them early - even if you feel better after a week, keep going for the full course.2. Saline Nasal Irrigation
Saltwater rinses (like neti pots or squeeze bottles) are simple, safe, and effective. They flush out irritants, moisturize dry nasal passages, and reduce swelling. A 2022 review found that 60% of patients using saline irrigation during withdrawal reported noticeable relief. Use it 2-3 times a day, especially in the morning and before bed. Warm salt water is gentler than cold.3. Short-Term Oral Steroids (for Severe Cases)
If your congestion is extreme - you’re waking up gasping, can’t sleep, or have lost your sense of smell - your doctor might prescribe a short 5-day course of prednisone. A 2021 trial showed 82% of patients improved significantly with this approach. This isn’t for everyone, but it’s a powerful tool for breaking the cycle fast.4. Avoid Oral Decongestants Too
Pseudoephedrine (Sudafed) and phenylephrine pills might seem like a good alternative. But they can make things worse. They constrict blood vessels everywhere - not just in your nose. That can raise your blood pressure. One study found 1 in 7 people with high blood pressure had dangerous spikes when using these pills. If you have heart issues or hypertension, skip them entirely.What Doesn’t Work - And Why
There are a lot of myths out there. Here’s what to avoid:- Switching brands: All OTC decongestant sprays work the same way. Switching from Afrin to a “natural” version doesn’t help - if it contains oxymetazoline, it’s the same problem.
- Using it less often: “I’ll use it once a day instead of three times.” That still triggers rebound. The damage happens with repeated use, not frequency.
- Essential oils or steam: Steam might feel good temporarily, but it doesn’t fix the inflammation. Some oils can irritate your nasal lining even more.
- Waiting it out without support: If you just stop and do nothing, your symptoms will be worse, longer, and you’re more likely to relapse.
Success Stories and Pitfalls
Real people have beaten this. One Reddit user, “AllergySufferer89,” wrote: “After 3 weeks of Flonase and no Afrin, my nose finally cleared up - the first week was hell but worth it.” That first week? That’s the hardest part. Most people who succeed stick with the corticosteroid plan. Those who relapse usually stop too soon - or didn’t use the corticosteroid consistently. Cleveland Clinic’s data shows that patients who got proper counseling during withdrawal had a 7% relapse rate. Those who didn’t? 22%. Talking to a pharmacist or doctor makes a huge difference.How to Prevent It From Happening Again
Once you’re better, don’t go back to the same habits. Here’s how to protect yourself:- Use decongestant sprays for no more than 3 days - period.
- Start with saline rinses for congestion. They’re safe for daily use.
- If you have chronic congestion, see a doctor. You might have allergies, a deviated septum, or nasal polyps - all treatable with the right plan.
- Keep a symptom diary. If you notice congestion returning after using a spray, stop immediately.
- Ask your pharmacist: “Is this a decongestant spray?” Many people don’t realize what’s in the bottle.
When to See a Doctor
You don’t need to suffer through this alone. See a doctor if:- You’ve been using nasal sprays for more than 7 days
- Your congestion hasn’t improved after 2 weeks of stopping the spray
- You’re having trouble sleeping, eating, or breathing
- You notice nasal bleeding, crusts, or a foul smell
- You’ve tried everything and still can’t breathe
Rebound congestion isn’t your fault. It’s a well-documented side effect of a common over-the-counter product. But it’s fixable. The path isn’t easy - but it’s clear: stop the spray, use corticosteroids, rinse with salt water, and give your nose time to heal. Your breathing will thank you.
Can I use nasal decongestant sprays again after recovering from rebound congestion?
Yes - but only with extreme caution. Once your nose has healed, you can use decongestant sprays again for short-term relief during a cold or allergy flare-up. But never use them for more than 3 days in a row. Always treat them like an emergency tool, not a daily fix. If you find yourself reaching for them again for routine congestion, talk to your doctor. There are safer long-term options.
How long does it take for nasal congestion to improve after stopping the spray?
Most people see some improvement after 5-7 days, but full recovery can take 2-4 weeks. The worst symptoms usually peak between days 2 and 5. Using intranasal corticosteroids and saline rinses during this time can cut recovery time in half. If you don’t see any change after 4 weeks, see a doctor - you might have another underlying issue.
Are there any natural remedies that help with rebound congestion?
Natural remedies like steam, humidifiers, or essential oils may offer temporary comfort, but they don’t treat the inflammation causing the congestion. The only proven, science-backed treatments are intranasal corticosteroids and saline irrigation. Avoid products claiming to “cure” rebound congestion - they’re not backed by evidence and may contain hidden decongestants.
Can children get rebound congestion from nasal sprays?
Yes - and it’s more dangerous in kids. Nasal decongestant sprays are not recommended for children under 6. Even in older kids, rebound congestion can develop quickly. If your child has chronic congestion, talk to a pediatrician or ENT specialist. There are safer, age-appropriate treatments, including saline sprays and allergy medications.
Why do some doctors recommend stopping one nostril at a time?
Stopping in one nostril at a time helps you keep breathing through the other side while the affected side heals. This reduces the shock to your system and makes withdrawal more tolerable. Many patients find this method less overwhelming than stopping both sides at once. It’s not a cure - it’s a strategy to make the healing process easier.
Can rebound congestion cause permanent damage?
Long-term overuse can lead to permanent changes. Chronic inflammation can cause nasal polyps - small, noncancerous growths that block airflow. It can also thin the nasal lining, making it more prone to bleeding and infection. The longer you delay treatment, the higher the risk. That’s why early intervention - within the first 2 weeks of symptoms - gives you the best chance of full recovery.





December 23, 2025 AT 03:32 AM
This is why America needs to stop treating OTC meds like candy. If you can’t read a label that says 'Do not use more than 3 days,' you shouldn’t be allowed near a pharmacy.
December 24, 2025 AT 02:15 AM
I was stuck in this cycle for 18 months. I thought I was just getting sicker every winter. Turns out, I was poisoning my own nose. Started Flonase, went cold turkey on Afrin - day 4 was brutal, like my sinuses were on fire. But by day 10? I could breathe through my nose for the first time in years. Worth every second of misery. Don’t give up.
December 24, 2025 AT 18:57 PM
It is not merely a matter of pharmacological dependence; it is a systemic failure of public health literacy. The over-the-counter availability of vasoconstrictive nasal agents constitutes a regulatory lacuna that permits the proliferation of iatrogenic pathology. The FDA warning labels are insufficiently prominent, and consumer education is catastrophically absent. One cannot reasonably expect laypersons to comprehend the pathophysiology of rebound congestion without formal medical training. This is not a personal failing - it is a societal one.
December 25, 2025 AT 04:49 AM
Oh, so now we’re blaming the patient for being misled by a bottle that says ‘for temporary relief’? The real tragedy is that doctors don’t warn people until it’s too late. I’ve had three patients in my clinic this month with this exact problem - all swore they ‘only used it once a day.’
December 26, 2025 AT 13:57 PM
wait… so u mean the stuff i’ve been using for 2 years is actually MAKING it worse?? like… the company is lying?? i thought it was just me being weak…
December 27, 2025 AT 04:34 AM
Big Pharma knows this is a cash cow. They don’t care if you’re addicted - they make billions off people cycling back for refills. The ‘3-day limit’ is buried in tiny font because they want you to keep buying. The FDA is bought and paid for. Look up the lobbying records. This isn’t medicine - it’s a trap.
December 27, 2025 AT 10:12 AM
Saline rinses changed my life. I used to be glued to my spray. Now I do a neti pot every morning - feels like a spa day for my sinuses. No chemicals, no addiction, no drama. Why didn’t anyone tell me this sooner? Also, try adding a pinch of baking soda to the salt. It’s gentler on the mucosa.
December 27, 2025 AT 10:59 AM
As a Canadian, I find it deeply concerning that American consumers are left to navigate such a complex medical issue without professional guidance. The lack of pharmacist-led intervention in OTC medication use is a structural flaw in your healthcare ecosystem. We mandate counseling for all nasal decongestants here - and our rates of rebound congestion are significantly lower.
December 28, 2025 AT 00:02 AM
…And yet, somehow, you still believe Flonase is ‘the solution’? Have you considered that corticosteroids suppress your immune system? That they’re just replacing one problem with another - one that’s slower, quieter, and more insidious? The real answer is to stop treating symptoms at all - and address the root cause: environmental toxins, EMF exposure, and glyphosate in your water. But no - you’ll just take another pill.
December 29, 2025 AT 14:44 PM
The strategy of tapering one nostril at a time is clinically sound and empirically supported. It mitigates the autonomic shock response associated with abrupt vasoconstrictor withdrawal. This approach aligns with principles of neuroplastic adaptation in mucosal vasculature and should be standardized in patient education materials. I recommend its inclusion in all primary care protocols.