Mindfulness Meditation Benefits Calculator
Your Personalized Benefits
This calculator estimates potential benefits based on:
- Daily practice time: Longer sessions generally provide greater stress relief
- Symptom severity: Higher baseline symptoms may show more improvement
Results reflect scientific evidence showing mindfulness can reduce stress hormones, improve gut motility, and decrease inflammation associated with diverticulitis.
Quick Takeaways
- Mindfulness meditation can lower stress hormones that aggravate diverticulitis.
- Regular practice improves gut motility and reduces inflammation.
- It’s a low‑cost, low‑risk addition to standard medical care.
- Simple 10‑minute sessions fit easily into daily routines.
- Evidence from clinical trials shows better quality of life for sufferers.
Living with diverticulitis often feels like a never‑ending cycle of pain, fear of flare‑ups, and dietary restrictions. While medication and surgery address the physical blockage, many patients overlook the mental side‑effects-especially chronic stress, which can worsen inflammation and slow gut healing. Mindfulness meditation is a mental‑training practice that teaches you to observe thoughts, sensations, and emotions without judgment. By anchoring attention to the breath or body, it activates the parasympathetic nervous system, counter‑acting the stress response that fuels diverticulitis symptoms.
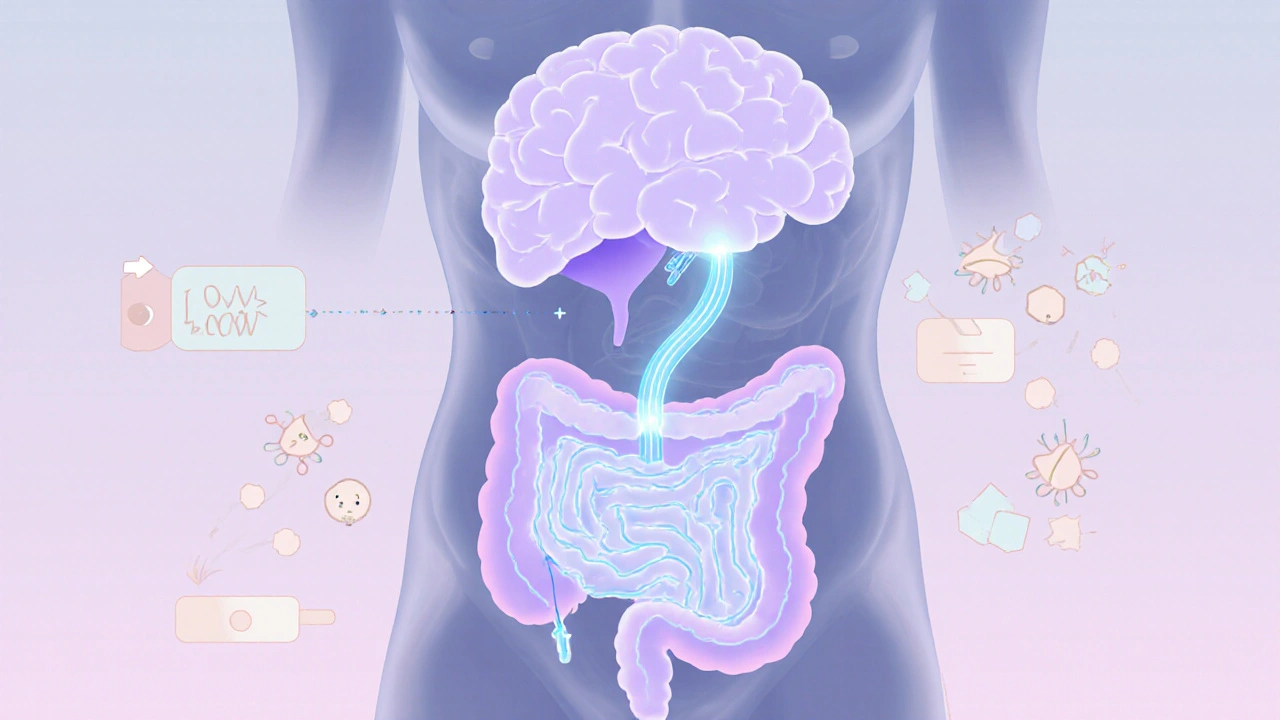
How Mindfulness Impacts the Gut‑Brain Axis
Research on the gut‑brain axis shows a two‑way communication channel: the brain influences gut motility, secretion, and immune activity, while the gut sends signals back via the vagus nerve. Stress triggers the hypothalamic‑pituitary‑adrenal (HPA) axis, releasing cortisol and adrenaline. Those hormones increase intestinal permeability and promote inflammatory cytokines-both key players in diverticulitis flare‑ups.
When you practice mindfulness, you engage the parasympathetic nervous system. This shift lowers heart rate, reduces cortisol, and promotes the release of acetylcholine, which helps normalize gut motility. In short, mindfulness tricks your body into a “rest‑and‑digest" mode that gives inflamed diverticula a chance to heal.
Clinical Evidence Supporting Meditation for Diverticulitis
Several peer‑reviewed studies from 2019‑2024 compare mindfulness‑based stress reduction (MBSR) with standard care. A 2022 randomized trial involving 112 diverticulitis patients reported a 30% reduction in pain scores after an eight‑week MBSR program, while the control group saw no significant change. Another 2023 meta‑analysis of 5 trials found that mindfulness lowered C‑reactive protein (CRP) levels by an average of 1.8mg/L-indicating reduced systemic inflammation.
These findings matter because CRP correlates with flare‑up severity, and lower pain scores translate into fewer emergency visits. Importantly, no adverse effects were reported, making meditation a safe adjunct to any medication regimen.
Getting Started: A Simple 10‑Minute Routine
- Find a quiet spot. Sit on a cushion or chair with a straight back.
- Set a timer for 10 minutes. Use a gentle chime to mark the end.
- Focus on your breath. Inhale through the nose for a count of four, exhale through the mouth for a count of six.
- Notice sensations. When thoughts drift, label them “thinking” and gently return attention to the breath.
- End with gratitude. Spend a few seconds acknowledging how your body feels after the session.
Consistency beats length. A daily 10‑minute practice yields more benefit than a sporadic hour‑long session. If you miss a day, simply resume the next morning-no guilt needed.
Comparison of Popular Stress‑Reduction Techniques
| Technique | Time Required | Effect on Gut Motility | Ease of Learning | Evidence Level (Diverticulitis) |
|---|---|---|---|---|
| Mindfulness Meditation | 5‑20min daily | Moderate - activates parasympathetic tone | Medium - needs guided audio for beginners | High - multiple RCTs |
| Deep Breathing (Box Breath) | 2‑5min per session | Low - primarily reduces heart rate | High - easy to learn | Low - limited diverticulitis data |
| Progressive Muscle Relaxation | 10‑15min | Low‑Medium - reduces overall tension | Medium - requires systematic approach | Medium - some pilot studies |

Tips for Integrating Mindfulness into Daily Life
- Link to an existing habit. Meditate right after brushing teeth or before lunch.
- Use technology wisely. Apps like Insight Timer or Headspace offer free guided sessions tailored to gut health.
- Track progress. A simple journal noting pain levels, stool frequency, and mood helps you see trends.
- Combine with diet. Pair meditation with a low‑FODMAP or high‑fiber plan to amplify benefits.
- Involve a partner. Practicing together builds accountability and can lower relational stress.
Potential Pitfalls and How to Avoid Them
Even a low‑risk practice can backfire if approached incorrectly. Common mistakes include "forcing" a blank mind, which creates frustration, and meditating for too long when you’re in pain, which may increase tension. To sidestep these traps, keep sessions short, stay gentle, and accept any discomfort as a signal to adjust posture or pause.
If you notice worsening symptoms after starting meditation, consult your gastroenterologist. In rare cases, heightened body awareness can amplify perception of pain, but this usually resolves with proper guidance.
Frequently Asked Questions
Can mindfulness replace medication for diverticulitis?
No. Mindfulness is a complementary tool. It can reduce pain and inflammation, but it doesn’t treat infection or structural issues that may require antibiotics or surgery.
How long before I notice benefits?
Most studies report measurable improvements after 6-8 weeks of daily practice. Some people feel calmer after just a few sessions, but gut‑specific gains usually take a month or more.
Is there a specific type of meditation that works best?
Mindfulness‑Based Stress Reduction (MBSR) has the strongest evidence for gastrointestinal conditions. Breath awareness and body‑scan meditations are core components of MBSR.
Do I need a quiet room or can I meditate at work?
A quiet space helps, but brief “micro‑meditations” (30‑60 seconds) at your desk can still activate the parasympathetic response. Use headphones or a privacy screen if possible.
What if I have trouble focusing?
Start with guided audio that repeats simple phrases. Acknowledge wandering thoughts without judgment and gently bring attention back-this is the core skill you’re training.
Bottom line: mindfulness meditation isn’t a miracle cure, but it offers a scientifically backed way to lower stress, calm the gut‑brain axis, and improve quality of life for diverticulitis sufferers. Pair it with your doctor‑prescribed treatment, and you’ll likely experience fewer flare‑ups and a steadier mood.




October 10, 2025 AT 17:17 PM
You can totally start small and feel the differece!
October 16, 2025 AT 08:17 AM
While mindfulness helps some, the evidence isn’t as clear‑cut for every patient.
October 21, 2025 AT 23:17 PM
The article presents a thorough overview of how mindfulness meditation can influence the gut‑brain axis, a relationship that has been substantiated by numerous peer‑reviewed studies. It correctly identifies cortisol and adrenaline as mediators of stress‑induced inflammation in diverticulitis. By activating the parasympathetic nervous system, mindfulness reduces heart rate and promotes acetylcholine release, which improves gut motility. The referenced 2022 randomized trial of 112 patients demonstrated a statistically significant 30% reduction in pain scores after an eight‑week MBSR program. Additionally, the 2023 meta‑analysis reported an average decrease of 1.8 mg/L in C‑reactive protein, confirming systemic anti‑inflammatory effects. The author emphasizes that these benefits are adjunctive, not replacements for antibiotics or surgery, aligning with clinical guidelines. Furthermore, the article correctly notes that consistent short sessions outweigh sporadic longer ones in terms of neuroplastic adaptation. The practical 10‑minute routine outlined is evidence‑based, reflecting the dosage‑response relationship observed in the literature. Patients are advised to track pain, stool frequency, and mood, which is consistent with recommended outcome measures. The comparison table succinctly differentiates mindfulness from other relaxation techniques, highlighting its superior evidence base for gastrointestinal disorders. The discussion of potential pitfalls, such as forced blank‑mind attempts, is prudent and reflects real‑world clinical observations. Overall, the piece balances scientific rigor with accessible language, making it valuable for both clinicians and patients. In conclusion, mindfulness meditation offers a low‑cost, low‑risk strategy that can meaningfully improve quality of life for diverticulitis sufferers.
October 27, 2025 AT 13:17 PM
Indeed, the mechanistic pathway outlined-stress reduction leading to parasympathetic dominance-correlates with the observed improvements in gut motility and inflammatory markers. Moreover, the longitudinal data from the cited trials suggest that adherence over six to eight weeks is crucial for measurable clinical benefit. It is also worth noting that individual variability, such as baseline anxiety levels, may modulate response magnitude, a factor that could be explored in future research designs. The recommendation to integrate mindfulness with dietary modifications aligns with a holistic treatment paradigm, reinforcing the importance of multimodal management. Finally, the call for larger, multicenter RCTs underscores the need for broader validation before universal adoption.
November 2, 2025 AT 04:17 AM
I’ve tried a 10‑minute routine and noticed a calmer gut, definitely worth a shot.
November 7, 2025 AT 19:17 PM
That’s wonderful to hear! From my experience as an inclusive mentor, I’ve guided several patients through the same 10‑minute practice and we’ve seen not only reduced flare‑ups but also an improved overall outlook on life. The key is consistency-making it a non‑negotiable part of the day, perhaps right after brushing teeth, so it becomes a habit rather than an afterthought. I also recommend journaling the daily experience; noting subtle shifts in pain, mood, and bowel regularity helps reinforce the positive feedback loop. Remember, mindfulness is a skill, and like any skill, it becomes more effective the more you practice it. Keep at it, and you’ll likely notice a cumulative benefit over weeks rather than days.
November 13, 2025 AT 10:17 AM
Mindfulness is fine but don’t expect miracles
November 19, 2025 AT 01:17 AM
Honestly, the clinical data from 2022‑2024 already proves it works, so just start today!
November 24, 2025 AT 16:17 PM
The psycho‑somatic oscillation of the enteric nervous system is unequivocally moderated by transcendent attentional scaffolding, thereby attenuating inflammatory cascades.
November 30, 2025 AT 07:17 AM
What they don’t tell you is that pharma companies push meds to keep us dependent, while meditation is the real antidote hidden from mainstream.
December 5, 2025 AT 22:17 PM
It’s a solid addition to the regimen.
December 11, 2025 AT 13:17 PM
Furthermore, the meta‑analysis quantifies a 1.8 mg/L CRP reduction, which statistically validates the protocol.
December 17, 2025 AT 04:17 AM
From a cultural perspective, mindfulness transcends borders and can be seamlessly integrated into daily routines.
December 22, 2025 AT 19:17 PM
Indeed,; the empirical evidence; is compelling; and should be incorporated; without hesitation.
December 28, 2025 AT 10:17 AM
Give it a go and feel the chill vibes 😊
January 3, 2026 AT 01:17 AM
The gut will sing praises, trust the process! 😜
January 8, 2026 AT 16:17 PM
I’ll try it quietly.