When you hear "generic drug," you probably think of a cheaper version of your prescription pill-same active ingredient, same effect, lower price. But what about biosimilars? If you’ve been told your doctor is switching you from a brand-name biologic to a "biosimilar," you might be confused. Are they just generics for fancy drugs? The answer is no-and that difference matters more than you think.
What Exactly Is a Generic Drug?
Generic drugs are exact chemical copies of brand-name medications. Take ibuprofen, for example. The brand-name version might be Advil, but the generic is chemically identical: same molecule, same structure, same dosage. Once the patent expires, any manufacturer can make it using the same formula. The FDA requires them to prove they work the same way in the body-same absorption rate, same strength, same side effects. That’s called bioequivalence.Because the chemistry is simple, making generics is cheap. It costs about $2 million to $5 million to develop one. That’s why they’re typically 40% to 50% cheaper than the original. In the U.S., generics make up 90% of all prescriptions filled-but only 20% of total drug spending. That’s the power of simplicity.
What Makes a Biosimilar Different?
Biosimilars are not chemical copies. They’re copies of biologic drugs-medicines made from living cells. Think of them like a hand-knitted sweater versus a factory-made one. Even if two sweaters look identical, the stitches, yarn tension, and texture might vary slightly. That’s how biosimilars work.Biologics, like Humira or Enbrel, are large proteins-sometimes thousands of times bigger than a regular drug molecule. They’re grown in living cells (like yeast or hamster ovary cells), not synthesized in a lab. Tiny changes in temperature, pH, or cell culture during production can alter the final product. That’s why biosimilars can’t be exact copies. They’re "highly similar"-with no clinically meaningful differences in safety or effectiveness, according to the FDA.
Developing a biosimilar isn’t just copying a recipe. It’s reverse-engineering a complex biological process you don’t fully understand. The original manufacturer keeps their exact method secret. So biosimilar makers have to build their own cell lines, their own purification steps, their own quality controls. They run over 200 analytical tests to prove similarity. Then they do animal studies and sometimes small clinical trials. All this costs $100 million to $200 million per product.
Regulatory Pathways: Why One Is Easier Than the Other
The FDA approved generics under the Hatch-Waxman Act of 1984. All they needed to show was bioequivalence: their drug enters the bloodstream at the same rate and amount as the brand. No new clinical trials needed.Biosimilars follow a different path-created by the Biologics Price Competition and Innovation Act (BPCIA) of 2009. The FDA doesn’t just check blood levels. They look at structure, function, purity, stability, immunogenicity (how likely it is to trigger an immune reaction), and sometimes clinical outcomes. The process is longer, more complex, and more expensive.
As of November 2023, the FDA has approved 42 biosimilars. Over 10,000 generic drugs are on the market. That’s not because biosimilars are less useful-it’s because they’re harder to make.

Can Pharmacists Switch You Automatically?
This is where things get personal. If your doctor prescribes a generic, your pharmacist can swap it in without telling you-because it’s identical. All 50 states allow this automatic substitution.With biosimilars? Not so fast. Only biosimilars designated as "interchangeable" can be swapped without the doctor’s approval. And as of 2023, only 7 out of 42 FDA-approved biosimilars have that status. The rest? You need a new prescription if your doctor wants you to switch.
Why the caution? Because even tiny differences in biologics can trigger immune responses. For someone with rheumatoid arthritis or Crohn’s disease, an unexpected immune reaction could mean a flare-up, hospital visit, or worse. Experts like the American Society of Health-System Pharmacists warn that biosimilars aren’t automatically interchangeable-unlike generics.
Cost Savings: What You Actually Pay
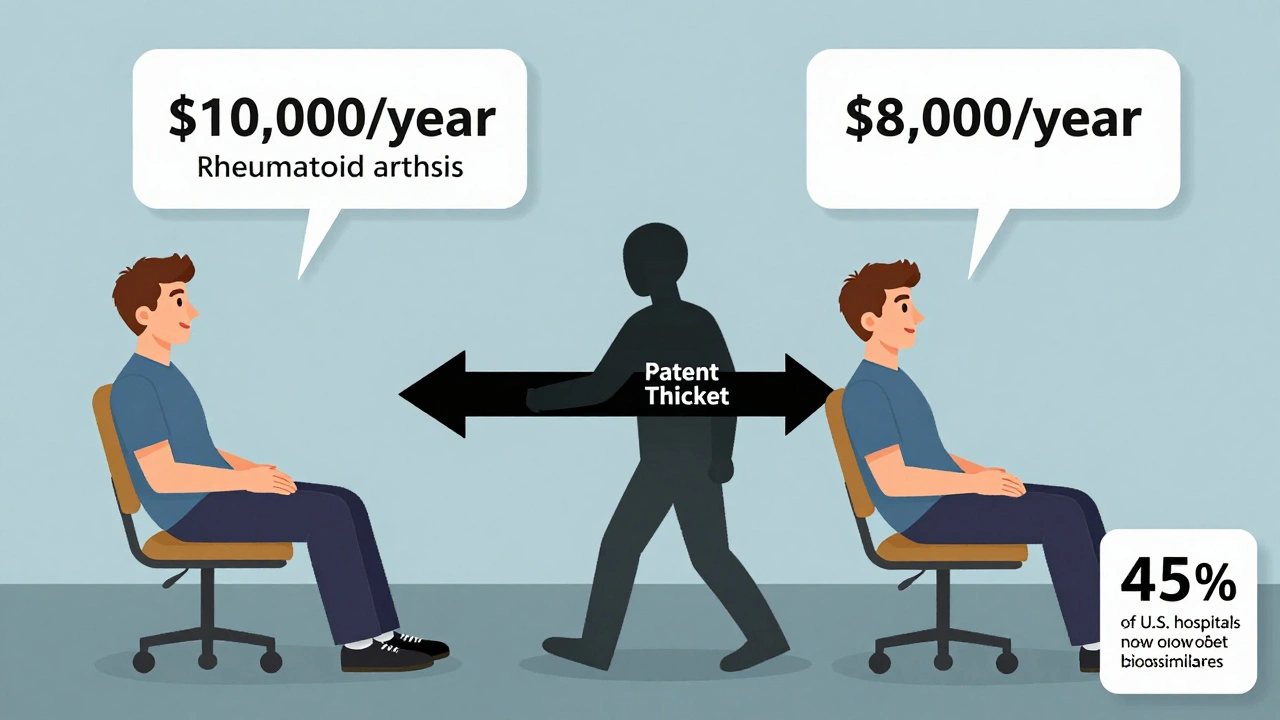
Generics save you a lot. If your brand-name pill costs $100, the generic might be $40. That’s a 60% drop.Biosimilars? They’re cheaper than the original biologic-but not by as much. Savings are typically 15% to 20%, though some reports say up to 33%. Why the smaller discount? Because development costs are so high. The manufacturer still needs to recoup $150 million in R&D. Plus, the original biologic maker often fights back with patent lawsuits-like AbbVie did with Humira, filing over 240 patents to delay competition.
But here’s the real story: even a 20% savings on a $10,000-a-year biologic drug means $2,000 saved per patient. That adds up fast in Medicare and private insurance. That’s why hospitals and specialty pharmacies are adopting biosimilars faster than you might expect. As of 2023, 45% of U.S. hospitals use at least one biosimilar.
Where Are They Used?
Generics are everywhere: antibiotics, blood pressure pills, antidepressants, pain relievers. They’re the backbone of affordable medicine.Biosimilars are focused on high-cost, complex conditions:
- Oncology: Trastuzumab (for breast cancer), bevacizumab (for colon cancer)
- Autoimmune diseases: Adalimumab (Humira), etanercept (Enbrel), infliximab (Remicade) for rheumatoid arthritis, psoriasis, Crohn’s
- Endocrinology: Insulin glargine for diabetes
These are not drugs you take for a few days. People stay on them for years. That’s why switching safely matters.
What Do Experts Say?
Dr. Gary Gibbons from the National Heart, Lung, and Blood Institute put it plainly: "Biosimilars require a fundamentally different regulatory approach than generics."The FDA is clear: "Biosimilars are not generics."
And Dr. Rachel B. Ballow, a pharmaceutical scientist, explains: "Because each reference product’s manufacturing process is proprietary, the biosimilar product always differs slightly from the reference product. This is in contrast to generic medications, which are identical."
Some critics argue the cost savings don’t justify the complexity. But the European Medicines Agency (EMA) has embraced biosimilars more aggressively. In Europe, they make up 35% of the biologics market-far higher than the under 3% in the U.S. That’s changing. With major biologics like Stelara and Eylea losing patent protection soon, biosimilar use is expected to jump to 25-30% of the U.S. market by 2028.
What Should You Do?
If your doctor suggests switching from a brand-name biologic to a biosimilar:- Ask if it’s an "interchangeable" biosimilar.
- Find out if your insurance requires prior authorization.
- Ask about monitoring-especially if you’ve been stable on the original drug.
- Don’t assume it’s the same as switching to a generic.
If you’re prescribed a generic? You can usually switch without worry. The FDA says they’re therapeutically equivalent. Your body will react the same way.
The bottom line: both generics and biosimilars help make medicine affordable. But they’re not the same. One is a mirror image. The other is a close cousin-similar in function, but made differently, regulated differently, and handled differently.
Knowing the difference isn’t just academic. It’s how you make smart choices about your treatment.
Are biosimilars safe?
Yes. The FDA requires biosimilars to show "no clinically meaningful differences" in safety, purity, and potency compared to the original biologic. This includes extensive testing for immune reactions, which is a major concern with biologics. Thousands of patients have used biosimilars for years without increased risks. However, because they’re not identical, switching from the original product should be done under medical supervision-especially for chronic conditions like rheumatoid arthritis or Crohn’s disease.
Can I get a biosimilar instead of my brand-name drug without asking my doctor?
Only if the biosimilar has been designated as "interchangeable" by the FDA. As of 2023, only 7 out of 42 approved biosimilars have that status. For all others, your pharmacist must get a new prescription from your doctor before switching you. This is different from generics, which can be automatically substituted in all 50 states.
Why are biosimilars more expensive to make than generics?
Biosimilars are made from living cells, not chemicals. That means the manufacturing process is far more complex. The original manufacturer’s exact method is secret, so biosimilar makers must develop their own cell lines, purification steps, and quality controls. They run over 200 analytical tests and often need animal and clinical studies. This can cost $100 million to $200 million. Generic drugs, by contrast, are chemically identical and cost only $2 million to $5 million to develop.
Do biosimilars work as well as the original biologic?
Yes, when approved by the FDA. Clinical trials show biosimilars produce the same results in terms of effectiveness, safety, and side effects as the original biologic. The FDA’s standard is "no clinically meaningful differences." That means if your doctor says the original works for you, the biosimilar should work just as well. But because they’re not identical, some doctors prefer to start new patients on biosimilars rather than switch those already stable on the brand-name drug.
Why aren’t more biosimilars available in the U.S.?
Three main reasons: high development costs, patent thickets (like AbbVie’s 240+ patents on Humira), and reimbursement challenges. Many insurers and hospitals still favor the original biologic because of how they’re paid ("buy-and-bill" models). Also, provider hesitancy exists due to concerns about immunogenicity and switching. But with major biologics like Stelara and Eylea losing patent protection soon, the number of available biosimilars is expected to rise sharply by 2028.



December 5, 2025 AT 05:45 AM
Biosimilars aren't just generics with a fancy name-they're like trying to copy a symphony by listening to a recording while blindfolded. The original isn't just a formula, it's a living process. And yeah, that's why they cost a fortune to make.
December 6, 2025 AT 11:19 AM
it's wild how we treat these two types of drugs like they're the same. they're not. one's a photocopy, the other's a hand-drawn replica. both work, but one's way more fragile.
December 6, 2025 AT 19:45 PM
Let me be perfectly clear-this entire discussion is a testament to the grotesque commodification of human biology under late-stage capitalism. The FDA's regulatory framework is a bureaucratic farce designed to appease pharmaceutical oligarchs who profit from obfuscation. Biosimilars are not 'similar'-they are approximations of approximations, built upon proprietary black boxes that no independent scientist can fully audit. And yet we are told to trust them? With our lives? With our immune systems? This is not medicine-it's pharmaceutical roulette with a side of insurance red tape.
December 7, 2025 AT 03:32 AM
my pharmacist swapped my Humira for a biosimilar last year. no issues. still feel fine. just wish more people knew the difference before panicking.
December 8, 2025 AT 02:11 AM
Why does America let foreign companies make our biosimilars while we sit around waiting for patent lawsuits to resolve? In China they’re building entire biosimilar factories in five years. We’re still debating whether a biosimilar is ‘interchangeable’ because lawyers got more power than scientists. This isn’t innovation-it’s surrender.
December 9, 2025 AT 08:58 AM
It’s interesting how both generics and biosimilars serve the same goal-accessibility-but require completely different approaches. One is about replication, the other about re-creation. Maybe that’s the real lesson here: not everything that’s similar is the same, and not everything that’s different can’t be trusted.
December 9, 2025 AT 09:44 AM
you people act like biosimilars are some dangerous experiment. bro, they’ve been used in europe for 15 years. if they were gonna kill people, we’d know by now. stop being scared of science because you don’t understand the word ‘protein’.
December 9, 2025 AT 10:45 AM
if your doctor suggests a biosimilar, don’t panic. ask questions. but also trust the science. you’ve got this 💪
December 9, 2025 AT 23:24 PM
One must consider the epistemological implications of regulatory approval in pharmaceuticals: if a biosimilar demonstrates no clinically meaningful difference, yet remains structurally distinct, does it not challenge the very notion of therapeutic equivalence as a metaphysical construct? The FDA’s reliance on statistical non-inferiority rather than ontological identity reveals a fundamental flaw in our medical episteme
December 10, 2025 AT 20:08 PM
theyre lying about biosimilars. the real reason theyre pushing them is so the gov can track you through your meds. the chips are in the packaging dont believe the hype
December 11, 2025 AT 02:34 AM
In my country, we have seen biosimilars reduce the burden on public health systems significantly. The key is transparent regulation and physician education. Patients must be informed, not frightened. Science, when properly communicated, does not need fear to be trusted.
December 12, 2025 AT 19:42 PM
People are dying because they’re being switched to these cheap knockoffs while Big Pharma laughs all the way to the bank. This isn’t healthcare-it’s a corporate massacre disguised as cost-saving. And you’re just sitting here like it’s normal. Wake up.