When you’ve been on a biologic drug for years - maybe infliximab or adalimumab - and your doctor says it’s time to switch to a biosimilar, it’s normal to feel uneasy. You’re not changing pills. You’re switching a complex, living medicine that’s been keeping your inflammation under control. What happens when you make that switch? Does it work the same? Will you feel worse? Or worse yet - will your disease flare up?
What Exactly Is a Biosimilar?
A biosimilar isn’t a generic. Generics are exact copies of simple chemical drugs like ibuprofen or metformin. Biosimilars are copies of biologic drugs - huge, complex molecules made from living cells. Think of it like trying to recreate a handmade Swiss watch using the same blueprints. Even with identical instructions, slight differences in materials or craftsmanship can happen. But here’s the key: regulatory agencies like the FDA and EMA require biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the original. That means if your disease is stable, switching shouldn’t change your outcomes.
The first biosimilar approved in the U.S. was Zarxio (filgrastim-sndz) in 2015. Since then, 37 biosimilars have been approved, mostly targeting inflammatory diseases like rheumatoid arthritis, psoriasis, and Crohn’s disease. The biggest players? TNF inhibitors - drugs like infliximab and adalimumab. These account for about 70% of all biosimilar use today.
Switching from Originator to Biosimilar: What Does the Data Say?
Over 80 studies - including 32 randomized trials and 48 real-world observations - have looked at what happens when patients switch from originator biologics to biosimilars. The results? Consistently reassuring.
In the NOR-Switch study, 481 patients with rheumatoid arthritis, psoriatic arthritis, or inflammatory bowel disease were randomly assigned to either stay on originator infliximab or switch to the biosimilar CT-P13. After one year, 60% of those on the originator were still on treatment. So were 52.6% of those who switched. The difference? Not statistically significant. No spikes in serious side effects. No surge in antibodies that attack the drug. No drop in drug levels in the blood.
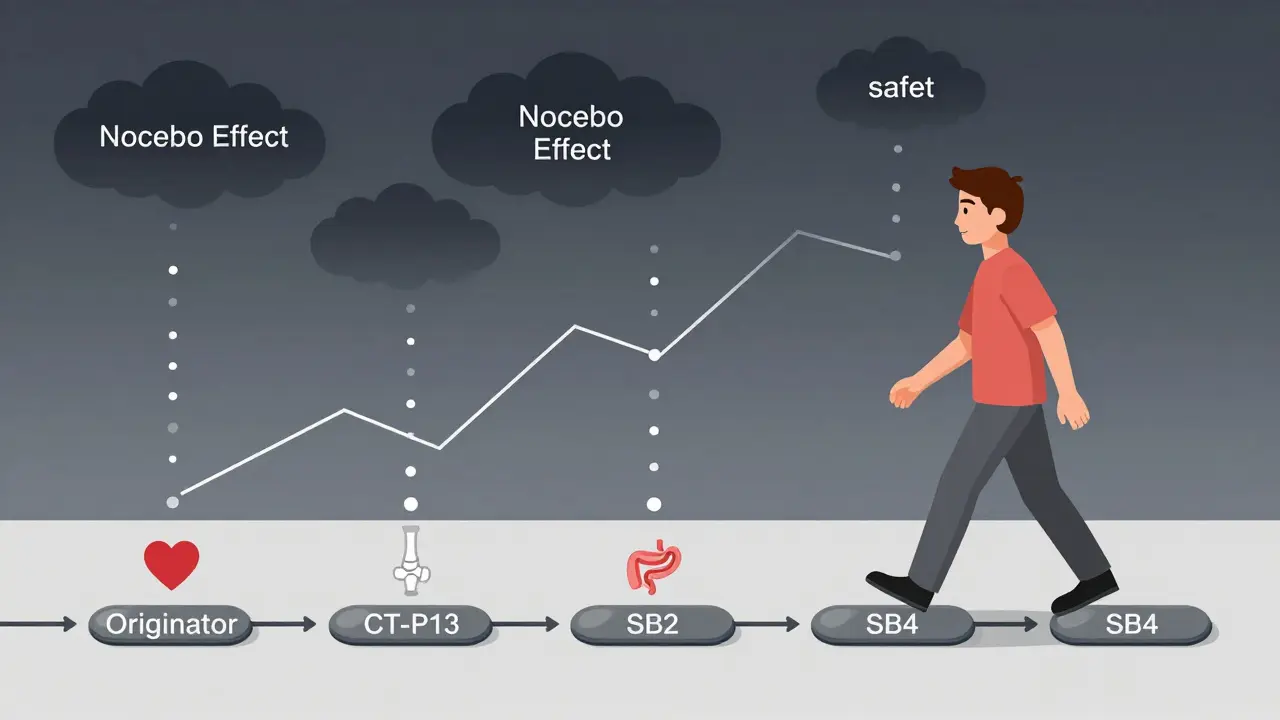
Another study tracked 140 patients who switched twice - from originator infliximab to CT-P13, then to another biosimilar, SB2. After both switches, drug levels stayed steady (around 4.1-4.3 μg/mL). Immunogenicity - the body making antibodies against the drug - was rare: only 3 cases per 100 patient-years. That’s lower than the annual flare rate for many chronic conditions.
For IBD patients switching from CT-P13 to SB2, 90.6% stayed in remission. Fecal calprotectin - a marker of gut inflammation - didn’t budge. In psoriasis, one-year retention rates for biosimilar adalimumab were nearly identical to the originator: 79% vs. 81.3%. Even in large population studies, there’s no evidence of increased risk for hospitalizations, infections, or death after switching.
Why Do Some People Stop Taking Their Biosimilar?
If the science says it’s safe, why do 4-18% of patients discontinue after a switch? The answer isn’t always medical. It’s psychological.
Studies show that patients who are told they’re being switched to a "cheaper version" - especially without proper explanation - are more likely to report new symptoms. This is called the nocebo effect: expecting something to go wrong makes you feel it. One study found 32.7% of patients reported new or worsening symptoms after a non-medical switch - even though their lab results and disease scores showed no change.
On Reddit, in forums like r/rheumatoidarthritis, hundreds of patients describe feeling "different" after switching. They say their joints ache more, their skin flares, or they get more tired. But when doctors check their DAS28 scores or PASI scores - the real clinical measures - there’s often no objective deterioration. The feeling is real. The cause? Likely anxiety, not the drug.
Real drug-related issues? They’re rare. Injection site reactions happen in about 7.8% of adalimumab biosimilar users. But true immunogenicity - where the body attacks the drug and it stops working - occurs in fewer than 2 out of every 100 patients per year. That’s about the same rate as with the originator.

Switching Between Biosimilars: Is It Safe?
Now, what if you switch from one biosimilar to another? Say you’re on CT-P13, and your insurance changes to SB2. Is that okay?
The data says yes - but with more caution. Studies show retention rates drop slightly compared to switching from originator to biosimilar. One Spanish study found 15.3% of IBD patients stopped their new biosimilar after switching from CT-P13 to SB2, compared to 8.7% in a control group. But here’s the twist: drug trough levels stayed the same. Inflammation markers didn’t rise. So why did they stop? Possibly because they were told they were being switched again - and the nocebo effect kicked in a second time.
Other studies, like one in Germany with 100 patients switching from SB4 to GP2015, showed 90% retention with no change in disease activity. So the results aren’t uniform. The difference? How the switch was handled. Patients who were prepared, informed, and monitored did far better.
Cost and Access: The Real Reason for Switching
Biosimilars cost 15-35% less than originators. In 2023, Humira biosimilars launched at a 35% discount. That’s billions saved for insurers and governments. In Europe, 67% of filgrastim use is now biosimilar. In the U.S., it’s only 24% - partly because of complex rebate systems and patent protections that delay competition.
But cost isn’t just about money. It’s about access. Many patients couldn’t afford the originator at all. Biosimilars open the door. In Australia, where biosimilars are widely adopted, more patients with autoimmune diseases are getting treatment than ever before. Without biosimilars, the healthcare system would be forced to ration these life-changing drugs.
What Makes a Safe Switch?
Not all switches are created equal. The difference between success and failure often comes down to three things: communication, monitoring, and timing.
- Communication: Patients need a 20-minute conversation - not a letter from their insurer. Explain that biosimilars aren’t "inferior." They’re proven. Show them the data. Answer their fears. The PERFUSE study showed that with good counseling, discontinuation dropped from 18% to just 6.4%.
- Monitoring: Don’t just switch and forget. Check disease activity at 3 months. Use DAS28 for arthritis, PASI for psoriasis, or fecal calprotectin for IBD. Measure drug levels if needed. Don’t assume a flare means the biosimilar failed - it might just be a natural progression.
- Timing: Switch when the disease is stable. Don’t switch during a flare, pregnancy, or if you’re about to have surgery. If you’ve had multiple drug failures before, proceed with extra care.
Doctors need to be trained in biologic monitoring. Pharmacists need to know how to explain switches. Insurance companies need to stop forcing switches without patient input.
Regulatory Differences: FDA vs. EMA
The U.S. and Europe handle biosimilars differently. The EMA says: if it’s a biosimilar, it’s switchable. No extra studies needed. The FDA requires extra data for a drug to be labeled "interchangeable" - meaning a pharmacist can swap it for the originator without asking the doctor. In 2024, Cyltezo became the first interchangeable adalimumab biosimilar in the U.S.
That’s a big deal. It means in some states, you might get a biosimilar at the pharmacy without even knowing - unless your doctor opts out. But it also means patients need to be even more informed. A switch you didn’t ask for can trigger anxiety - and nocebo effects.
What About Long-Term Safety?
The longest data we have comes from the NOR-SWITCH II extension. Patients who switched once - then switched again - were followed for two years. 89.2% stayed on treatment. No increase in serious infections. No rise in cancer rates. No unexpected side effects.
That’s powerful. It means switching isn’t just safe for one change. It’s safe for multiple switches. And with over $178 billion in biologic patents expiring by 2025, more switches are coming. The healthcare system isn’t going back.
Final Thoughts: Should You Switch?
If your disease is under control, and your doctor recommends switching - yes, you should. The science is clear: biosimilars work just as well. The risks are low. The benefits - lower cost, better access, more treatment options - are huge.
But don’t let fear make the decision for you. Ask questions. Get the facts. If you’re worried, ask for a 3-month follow-up. Track your symptoms. Don’t assume every ache or flare is the drug’s fault.
Switching isn’t a downgrade. It’s evolution. And for millions of people with chronic autoimmune diseases, it’s the difference between living with pain - and living well.





January 16, 2026 AT 01:39 AM
Been on Humira for 8 years and switched to the biosimilar last year. No difference in my skin or joints. I actually feel better because I’m not stressing about the bill anymore. Doctors need to stop treating us like we’re fragile.
January 17, 2026 AT 18:33 PM
They’re lying. Biosimilars are just knockoffs made in China with recycled lab equipment. My cousin’s friend got hospitalized after switching. They don’t tell you the real side effects. Big Pharma and the FDA are in bed together.
January 18, 2026 AT 20:10 PM
Man, I read this whole thing while sipping chai in Mumbai and I’m just blown away. In India, we’ve been using biosimilars for over a decade because the originals were just too expensive for most people. I know guys who’ve been on infliximab biosimilars since 2012 and they’re still hiking in the Himalayas. It’s not about cheap, it’s about access. If your body doesn’t reject it and your doctor monitors you, you’re golden. Stop fearing science because it’s not made in the US or Europe.
January 19, 2026 AT 06:32 AM
If your doctor switches you without a conversation, that’s malpractice. Not because the drug is bad, but because they disrespected your autonomy. You have a right to be informed, not just notified. Demand the 20-minute talk. If they refuse, find a new doctor.
January 20, 2026 AT 09:31 AM
The FDA’s definition of "interchangeable" is a bureaucratic farce. It’s not about clinical equivalence-it’s about cost-cutting disguised as innovation. The EMA’s approach is more honest: if it’s a biosimilar, assume it’s switchable unless proven otherwise. But the U.S. system rewards legal loopholes over patient trust. This isn’t progress. It’s corporate exploitation wrapped in medical jargon.
January 20, 2026 AT 19:26 PM
I switched last spring and felt weird for two weeks. My hands were stiff. I thought it was the drug. Then I realized I’d been sleeping worse because I was anxious about the switch. Once I stopped obsessing, the stiffness went away. It’s not the biosimilar. It’s the fear.
January 22, 2026 AT 00:39 AM
So let me get this straight. You’re telling me that a drug made by a different company, using different cell lines, in a different facility, with slightly different excipients, is functionally identical to the original… and we’re supposed to trust that because a regulatory agency says so? Fascinating. Tell me again how science is objective.
January 22, 2026 AT 21:33 PM
As a rheum nurse, I’ve seen this play out a hundred times. The nocebo effect is real and it’s brutal. Patients come in saying "I can’t breathe" after switching-only to find their O2 sat is 98% and their CRP is normal. It’s not the drug. It’s the narrative. We now give patients a one-pager with real data and a QR code to the NOR-Switch study. Discontinuation dropped 60% in our clinic. Knowledge is the antidote to fear.
January 23, 2026 AT 13:54 PM
My brother switched from Remicade to CT-P13 in Delhi. He was scared too. But we sat down, looked at the studies together, and he gave it a shot. Two years later, he’s still going strong. No flares. No extra costs. Just life. If you’re worried, talk to someone who’s been there-not the internet. Real stories matter more than headlines.
January 24, 2026 AT 16:08 PM
Cost savings are great but don’t pretend this isn’t a corporate power play. Insurance companies push biosimilars because they make more money. Patients get the short end. We need policy reform not just education. The system is rigged.
January 25, 2026 AT 18:21 PM
I switched twice-first from Humira to a biosimilar, then to another one. Felt fine both times. My rheumatologist said "we’ll check your levels in 3 months" and did. That’s the difference. If your doc just says "switch now" and leaves you hanging, that’s the problem. Not the drug.