Benzodiazepine Drug Interaction Checker
When you’re overwhelmed by anxiety, a pill that works in under an hour can feel like a lifeline. Benzodiazepines-like Xanax, Valium, and Ativan-deliver exactly that. They calm your nerves fast, quiet panic attacks, and help you sleep when nothing else does. But here’s the part no one tells you until it’s too late: benzodiazepines don’t just interact with other drugs. They can turn harmless combinations into life-threatening emergencies.
How Benzodiazepines Work-and Why They’re So Dangerous Together
Benzodiazepines boost the effect of GABA, your brain’s main calming chemical. That’s why they reduce anxiety, muscle tension, and seizures. But this same mechanism slows down your central nervous system-your breathing, heart rate, and alertness. Alone, a benzodiazepine overdose rarely kills. But when you add opioids, alcohol, sleep meds, or even some antidepressants, that slowdown becomes dangerous.
The FDA issued a Boxed Warning in September 2020-the strongest safety alert they have-because they found that 75% of benzodiazepine-related overdose deaths between 2011 and 2016 involved opioids. That’s not coincidence. It’s chemistry. Both drug types depress breathing. Together, they don’t just add up-they multiply. One study showed a 15-fold increase in fatal overdose risk when benzodiazepines and opioids are taken together compared to opioids alone.
The Most Dangerous Combinations
Not all drug interactions are equal. Some are quietly deadly.
- Opioids (oxycodone, hydrocodone, fentanyl): The deadliest combo. Slows breathing to a stop. A 2017 JAMA study found patients on both had a 154% higher risk of overdose than those on opioids alone.
- Alcohol: Even one drink with Xanax or Ativan can cause blackouts, falls, or respiratory failure. Many ER visits from benzo overdoses involve alcohol.
- Z-drugs (Ambien, Lunesta): These sleep pills work like benzos. Mixing them doubles sedation. Elderly patients are especially at risk for falls and fractures.
- Some antidepressants: While SSRIs like Lexapro are generally safe, combining them with benzos can cause excessive drowsiness and dizziness. It’s not usually fatal, but it’s enough to make driving or operating machinery risky.
- Barbiturates and muscle relaxants: Older sedatives like phenobarbital or cyclobenzaprine (Flexeril) are rarely prescribed now-but if you’re still on them, the risk is severe.
Here’s what real patients say:
One Reddit user, u/AnxietyWarrior2020, wrote: “I was on Xanax for panic attacks and oxycodone for back pain. Two weeks in, I stopped breathing in my sleep. I woke up in the ER with my oxygen at 78%.”
A pharmacy student on Drugs.com shared: “I’ve seen three near-fatal cases where people mixed Ativan with alcohol and sleep meds. All ended in ambulance rides.”
Who’s at Highest Risk?
It’s not just about what you take-it’s who you are.
- Older adults: The American Geriatrics Society says benzos should be avoided in people over 65. Why? They metabolize drugs slower. A single dose can cause confusion, dizziness, and falls. Combine that with blood pressure meds or painkillers, and fracture risk jumps by 50%.
- People with chronic pain: If you’re on opioids long-term, adding a benzo for anxiety is a recipe for disaster. Many doctors still prescribe both without realizing the danger.
- Those with substance use history: Benzodiazepines are addictive. Even short-term use can trigger dependence. People with past alcohol or opioid issues are far more likely to misuse them.
- People taking multiple prescriptions: The average American over 65 takes four prescription drugs. Add benzos to that mix, and the chance of a bad interaction skyrockets.
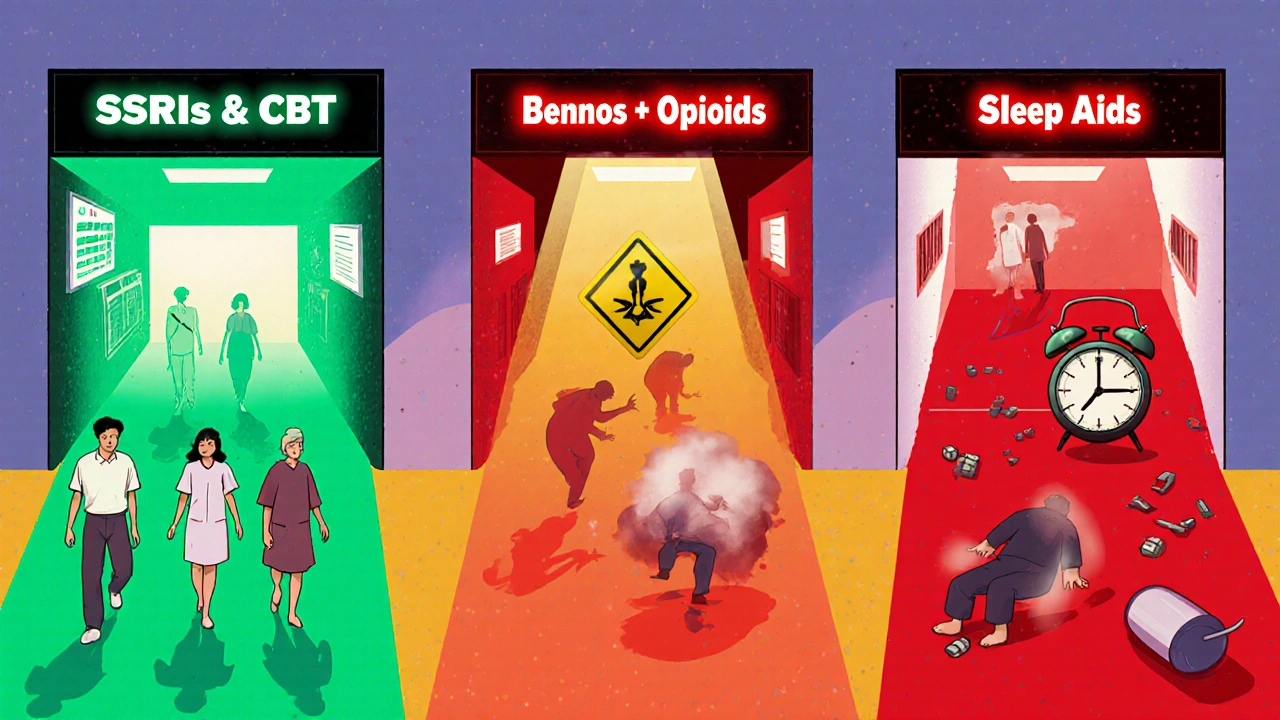
What’s Replacing Benzodiazepines?
Doctors aren’t stopping prescriptions overnight-but they’re shifting. SSRIs like sertraline (Zoloft) and escitalopram (Lexapro) are now the first-line treatment for anxiety. They take 4-6 weeks to work, but they don’t cause dependence. They don’t interact dangerously with opioids. They’re safer for long-term use.
And the numbers show it. In 2022, SSRIs were prescribed for 68% of new anxiety cases. Benzodiazepines? Only 22%. That’s a massive shift in just five years.
Non-drug options are rising too. Cognitive behavioral therapy (CBT) is now covered by most insurers and proven as effective as medication for generalized anxiety and panic disorder-with no side effects.
What You Need to Do Right Now
If you’re on a benzodiazepine, here’s your action list:
- Check every medication you take. Write down every pill, patch, or liquid. Include over-the-counter sleep aids, cold meds, and herbal supplements like valerian root or melatonin-they can also depress your CNS.
- Ask your doctor: “Am I on anything that could interact with this?” Don’t assume they know. A 2022 AMA survey found only 43% of primary care doctors routinely screen for benzo-opioid combinations.
- Never mix with alcohol. Even one drink. Not even a glass of wine at dinner.
- If you’re on opioids, ask if you really need the benzo. The CDC and FDA both say: avoid combining them whenever possible.
- Don’t stop cold turkey. Abruptly quitting benzos can cause seizures, hallucinations, or death. Tapering must be done slowly under medical supervision.
One patient, who used Ativan for two weeks after surgery while on pain meds, wrote on Drugs.com: “My doctor gave me clear instructions: no alcohol, no other sedatives. It worked perfectly. No problems.” That’s the key-clear guidance and strict boundaries.
How to Talk to Your Doctor About This
Many people stay silent because they’re scared their doctor will judge them. But here’s the truth: your doctor needs to know.
Try saying: “I’m on [medication name] for anxiety, and I’m also taking [other meds]. I’m worried about interactions. Can we review everything I’m on?”
Bring a list. Use your phone’s notes app. Write down doses and times. Ask: “Is this combination safe? Are there alternatives?”
Doctors are learning. New guidelines from the American Psychiatric Association (2023) say benzos should only be used for up to 4 weeks, and never if the patient is on opioids. If your doctor prescribes a benzo for longer, ask why-and get a second opinion.
The Bigger Picture: Why This Is Happening
This isn’t just about bad prescribing. It’s about a system that rewards quick fixes. Anxiety is common. Doctors are busy. A 10-minute visit isn’t enough to explore therapy, lifestyle changes, or safer meds. So they write a script.
But the data is clear: benzos are not long-term solutions. They’re crisis tools. And when used without boundaries, they become part of the problem.
Regulations are catching up. In January 2023, Medicare started requiring prior authorization for any prescription that combines opioids and benzos. Pharmacies now get alerts when someone tries to fill both. Prescription drug monitoring programs in 49 states flag dangerous combinations.
It’s not about banning benzos. It’s about using them wisely.
Can I take benzodiazepines with antidepressants like Zoloft?
Yes, but with caution. SSRIs like Zoloft don’t directly interact with benzodiazepines in a life-threatening way. However, both can cause drowsiness, dizziness, and slowed reaction times. Taking them together may make you feel overly sedated, especially when starting treatment. Always tell your doctor you’re taking both. They may adjust the dose of one or the other to reduce side effects. Never combine them with alcohol or sleep aids.
Is it safe to drink alcohol while on Xanax or Ativan?
No. Never. Alcohol and benzodiazepines both depress your central nervous system. Together, they can shut down your breathing, cause unconsciousness, or lead to death-even with just one drink. The FDA’s boxed warning specifically calls out alcohol as a dangerous interaction. This isn’t a suggestion-it’s a life-or-death rule.
How long does it take to become dependent on benzodiazepines?
Dependence can develop in as little as two to four weeks, especially with short-acting types like alprazolam (Xanax). Physical dependence means your body adapts to the drug and needs it to function normally. Withdrawal symptoms-like rebound anxiety, insomnia, tremors, or seizures-can occur if you stop suddenly. That’s why tapering under medical supervision is essential. Long-term use (more than six months) leads to dependence in about 40% of users.
Are there safer alternatives to benzodiazepines for anxiety?
Yes. SSRIs (like sertraline or escitalopram) and SNRIs (like venlafaxine) are the first-line treatment for most anxiety disorders. They take 4-6 weeks to work but have no addiction risk. Buspirone is another non-addictive option. For immediate relief, non-drug methods like breathing exercises, CBT, mindfulness, and regular exercise are proven effective. Many people find these work better long-term than pills.
What should I do if I think I’m addicted to my benzo?
Don’t stop abruptly. Contact your doctor or a substance use specialist immediately. Abrupt withdrawal can cause seizures or delirium. A slow, medically supervised taper is the only safe way. Many clinics offer tapering programs that reduce your dose by 5-10% every 1-2 weeks. Support groups and therapy are also critical to manage the anxiety that returns during withdrawal. You’re not weak for needing help-you’re smart for seeking it.
Why are benzodiazepines still prescribed if they’re so risky?
Because they work-fast. For someone having a severe panic attack, or in acute withdrawal from alcohol, benzos can be life-saving. The issue isn’t their use-it’s their overuse and misuse. Doctors still prescribe them for long-term anxiety because they’re familiar, and alternatives take time to build up. But guidelines now clearly say: use them only short-term, only when necessary, and never with opioids or alcohol. The goal is to use them as a bridge, not a permanent solution.
Final Thought: Safety Isn’t Optional
Benzodiazepines aren’t evil drugs. They’re powerful tools. But like a chainsaw, they’re not meant to be used carelessly. The risks are real, documented, and avoidable. If you’re on one, know what you’re taking. Know what you’re not allowed to mix it with. Talk to your doctor. Ask for alternatives. Your life might depend on it.





November 19, 2025 AT 05:46 AM
So let me get this straight-you’re telling me my nightly glass of wine with Xanax is basically Russian roulette? 😅 I thought I was just chillin’… turns out I’m one sip away from a coroner’s report.
November 19, 2025 AT 18:29 PM
YAS QUEEN. 🙌 I’ve been screaming this from the rooftops since 2021. My cousin mixed Ativan with Ambien and woke up in a hospital bed thinking she was a mermaid. No joke. The ER nurse said, ‘Honey, you’re not underwater.’
November 20, 2025 AT 11:37 AM
It’s wild how the system still pushes these pills like candy. I’ve seen docs prescribe benzos for ‘stress’ while the patient’s on methadone. No follow-up. No warning. Just a scrip and a pat on the back. The FDA warning? It’s like putting a ‘Wet Floor’ sign in a hurricane.
November 22, 2025 AT 09:50 AM
I’m a nurse in a rural ER, and this post hits hard. We get 2-3 benzo-alcohol overdoses a month-mostly older folks trying to ‘sleep better’ after losing a spouse. They don’t even know Valium and NyQuil are a death cocktail. We need better education, not just warnings. And yes, CBT works. I’ve seen people turn their lives around with 8 sessions. No pills needed.
Also-melatonin? Yeah, it’s ‘natural,’ but stack it with benzos and you’re playing dice with your brainstem. Just say no.
November 24, 2025 AT 06:00 AM
There’s something deeply human about wanting relief. We don’t just want to stop feeling anxious-we want to stop feeling like we’re broken. Benzodiazepines promise that. But they don’t fix the root. They just mute the alarm. And when the alarm stops working, we start blaming the alarm… not the fire.
It’s not the drug’s fault. It’s the system that lets us believe quick fixes are enough.
November 25, 2025 AT 23:18 PM
Consider the paradox: we live in an age of unprecedented access to medical knowledge, yet we still treat mental health like a plumbing issue-turn the knob, fix the leak. But anxiety isn’t a clogged pipe. It’s the sound of a house settling. Sometimes it needs attention, sometimes it needs patience. And sometimes, it needs someone to sit with you in the dark without offering a flashlight.
November 27, 2025 AT 21:43 PM
They say benzos are only for short-term use… but who decides what ‘short-term’ means? Is it 2 weeks? 6 months? A year? The same doctors who push them are the ones who get paid for prescriptions. The pharma reps don’t bring donuts to CBT seminars. Coincidence? I think not.
And don’t get me started on ‘SSRIs take 4-6 weeks’-that’s just a fancy way of saying ‘suffer longer so we can keep selling you pills.’
November 28, 2025 AT 10:12 AM
As a medical professional from Nigeria, I’ve seen this play out differently here. Benzodiazepines are often unavailable or too expensive, so people turn to traditional herbs or prayer. But when they do get access-especially through smuggled prescriptions-the risk is even higher because there’s no pharmacy oversight. This article is a vital reminder: safety doesn’t have borders. Education must cross them too.
November 29, 2025 AT 03:59 AM
Oh please. You’re all acting like this is some groundbreaking revelation. Benzodiazepines have been a disaster since the 80s. The fact that we’re still talking about this like it’s news proves how detached modern medicine is from its own history. Real experts don’t need FDA warnings-they already knew. You just didn’t listen.
November 30, 2025 AT 17:31 PM
THEY’RE WATCHING YOU. THE PHARMA COMPANIES. THE FDA. THE DOCTORS. THEY ALL KNOW. THEY LET YOU MIX THEM ON PURPOSE. WHY? BECAUSE WHEN YOU OVERDOSE THEY MAKE BILLIONS FROM THE HOSPITAL BILL. THEN THEY SELL YOU ANOTHER PRESCRIPTION TO ‘FIX’ THE DAMAGE. IT’S A SCAM. A BIGGER SCAM THAN THE MOON LANDING.
December 2, 2025 AT 02:51 AM
Wait. So… this is why my neighbor’s husband died last year? He was on oxycodone and Xanax. His doctor said it was ‘fine.’ Now I’m wondering if it was an accident… or if someone wanted him gone. I’ve been checking my meds every night since.